which symptoms would damage the spinal accessory nerve
The spinal accessory nerve, also known as cranial nerve XI, plays a crucial role in the movement and function of certain muscles in the head and neck. Damage to this nerve can result in various symptoms that can significantly affect a person’s quality of life. Understanding and recognizing these symptoms is essential for timely diagnosis and appropriate treatment. In this article, we will delve into the anatomy and function of the spinal accessory nerve, explore its potential causes of damage, discuss the symptoms that may arise as a result, analyze the diagnostic procedures used to identify the nerve damage, examine the available treatment options, and shed light on the prognosis and recovery outlook. However, it is important to remember that the information provided here is for educational purposes only, and medical advice should always be sought from a qualified healthcare professional.
Understanding the Spinal Accessory Nerve
The spinal accessory nerve, also known as the accessory nerve or cranial nerve XI, is a vital component of the nervous system. It plays a crucial role in enabling voluntary movements of the head and neck. Let’s delve deeper into the anatomy and function of this fascinating nerve.
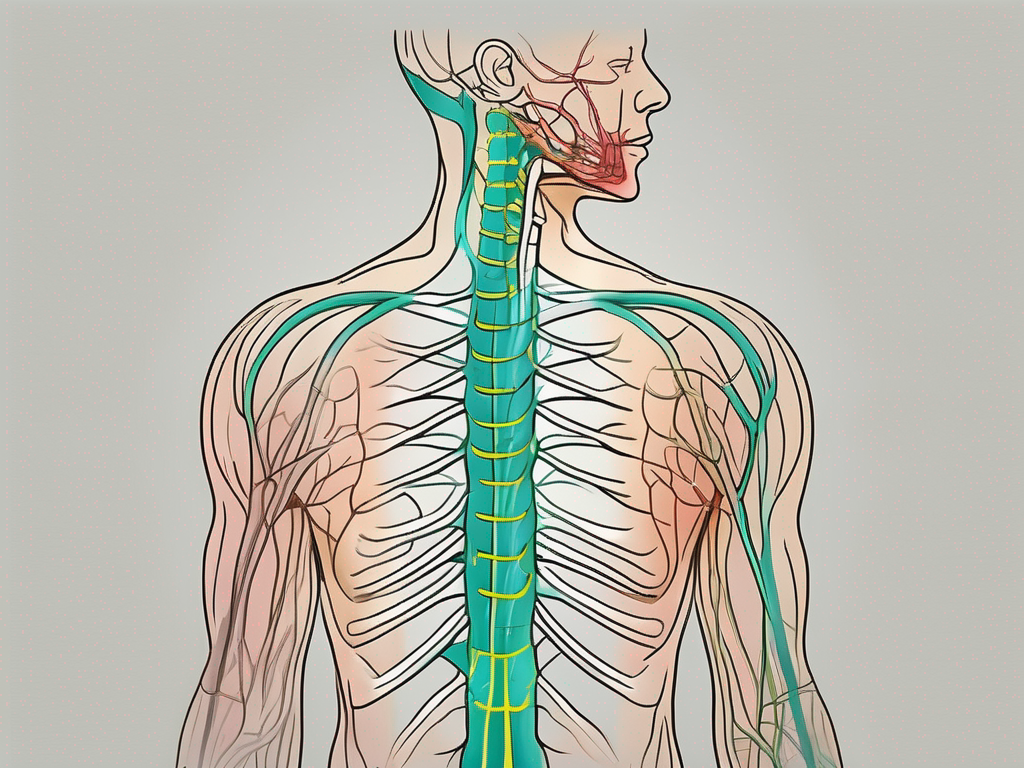
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve arises from the lower part of the brainstem, specifically the medulla oblongata. It consists of two distinct components: the cranial component and the spinal component.
The cranial component emerges from the medulla oblongata and primarily innervates the muscles involved in controlling the movement of the eyes and the soft palate. These muscles are essential for various functions such as eye movement coordination and swallowing.
On the other hand, the spinal component of the spinal accessory nerve originates from the upper spinal cord. It supplies the trapezius and sternocleidomastoid muscles, both of which are crucial for movements of the head and neck.
The trapezius muscle, innervated by the spinal component of the nerve, spans across the upper back and shoulders. It plays a significant role in shoulder movement, allowing us to perform actions such as lifting, rotating, and retracting the shoulders.
The sternocleidomastoid muscle, also innervated by the spinal component of the nerve, is located on the sides of the neck. It enables head rotation and flexion, allowing us to turn our heads from side to side and tilt them forward and backward.
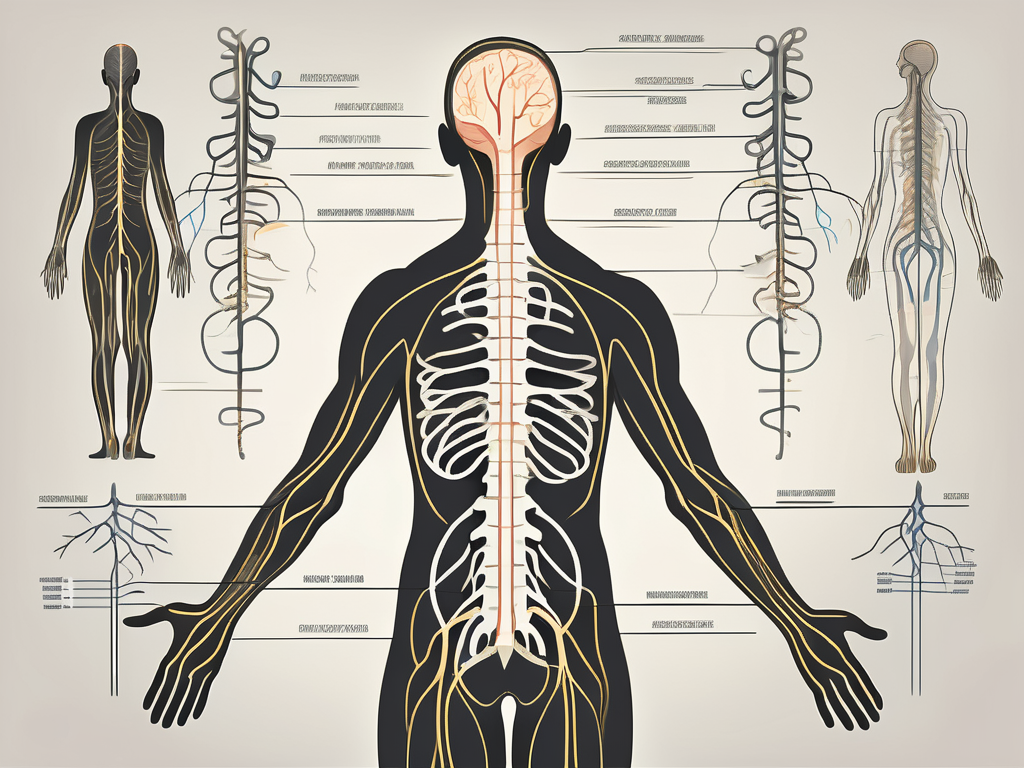
Function of the Spinal Accessory Nerve
The spinal accessory nerve is responsible for a wide range of voluntary movements of the head and neck. Its coordinated action with the trapezius and sternocleidomastoid muscles allows us to perform everyday activities with ease.
For instance, the combined action of the trapezius muscles on both sides of the body enables us to shrug our shoulders. This movement is essential for lifting objects, maintaining posture, and expressing emotions.
Meanwhile, the sternocleidomastoid muscles on either side of the neck work together to rotate the head. This enables us to look around, scan our environment, and engage in activities that require visual attention, such as driving or playing sports.
Furthermore, the spinal accessory nerve also plays a role in head flexion and extension. These movements are essential for various activities, including nodding, tilting the head backward to look up, or bringing the chin closer to the chest.
In summary, the spinal accessory nerve is a remarkable motor nerve that enables the voluntary movements of the head and neck. Its intricate connections with the trapezius and sternocleidomastoid muscles allow us to perform a wide range of actions, making it an indispensable component of our daily lives.
Potential Causes of Spinal Accessory Nerve Damage
Trauma and Injury
One of the most common causes of spinal accessory nerve damage is trauma or injury. Car accidents, falls, sports-related injuries, and physical assaults can all result in damage to the nerve. Trauma may occur due to direct impact or stretching of the nerve, leading to partial or complete disruption of its function. Prompt medical attention is crucial in cases of trauma to minimize the potential damage and facilitate recovery.
When it comes to trauma-related spinal accessory nerve damage, the severity of the injury can vary. In some cases, the nerve may only be partially affected, resulting in temporary weakness or limited mobility. However, more severe trauma can cause complete nerve disruption, leading to long-term or even permanent impairment.
Rehabilitation plays a vital role in the recovery process for individuals with spinal accessory nerve damage caused by trauma. Physical therapy and targeted exercises can help strengthen the surrounding muscles and improve overall function. Additionally, pain management techniques and assistive devices may be recommended to enhance the quality of life for those affected.
Surgical Complications
In some cases, surgical procedures in the head and neck region may inadvertently cause damage to the spinal accessory nerve. Surgeries such as lymph node removal, neck dissections, or procedures involving the posterior cranial fossa carry a risk of nerve injury. It is important for surgeons to exercise caution and meticulously plan and perform these operations to minimize the chances of nerve damage. Discussing potential risks and complications with the healthcare team before undergoing any surgery is essential.
When it comes to surgical complications, prevention is key. Surgeons must carefully assess the patient’s anatomy and plan the procedure accordingly to avoid unnecessary damage to the spinal accessory nerve. In complex cases, the use of advanced imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT), can aid in surgical planning and reduce the risk of nerve injury.
In the event that spinal accessory nerve damage occurs as a result of surgical complications, prompt identification and intervention are crucial. Nerve repair or reconstruction techniques may be employed to restore function and improve outcomes. Rehabilitation and physical therapy are often recommended to help patients regain strength and mobility in the affected area.
Neurological Disorders
Neurological disorders, such as tumors or infections affecting the brainstem or upper cervical spine, can also lead to spinal accessory nerve damage. These conditions may directly impact the nerve itself or result in compression by surrounding structures. Prompt identification and appropriate management of the underlying neurological disorder are crucial for minimizing nerve damage and optimizing recovery.
When it comes to neurological disorders, early diagnosis and treatment are essential. Timely intervention can help prevent further damage to the spinal accessory nerve and improve the overall prognosis. In some cases, surgical removal of tumors or targeted therapy for infections may be necessary to alleviate pressure on the nerve and promote healing.
Rehabilitation and supportive care are often integral components of the treatment plan for individuals with spinal accessory nerve damage caused by neurological disorders. Physical therapy, occupational therapy, and speech therapy may be recommended to address specific functional deficits and improve overall quality of life.
Identifying Symptoms of Spinal Accessory Nerve Damage
Physical Symptoms
Physical symptoms of spinal accessory nerve damage may manifest in different ways, depending on the specific muscles affected. Weakness or inability to move the head or shoulders properly may be observed. Individuals with spinal accessory nerve damage may experience difficulty shrugging their shoulders, rotating their head, or maintaining good posture. The impairment can significantly impact daily activities and overall functionality.
For example, individuals may find it challenging to lift heavy objects due to the weakened muscles in their shoulders. Simple tasks like reaching overhead to grab an item from a shelf can become a struggle. Additionally, the inability to rotate the head properly can affect one’s ability to check blind spots while driving or turning to engage in conversations.
Furthermore, maintaining good posture becomes a challenge for those with spinal accessory nerve damage. The muscles responsible for supporting the neck and upper back may weaken, causing individuals to slouch or experience discomfort when sitting or standing for extended periods.
Sensory Symptoms
Unlike some other cranial nerves, the spinal accessory nerve is primarily involved in motor function, meaning that sensory symptoms are less commonly associated with its damage. However, in some cases, individuals may experience alterations in sensations around the affected area. This can include numbness, tingling, or abnormal sensations in the neck or shoulder region. These sensory changes are typically secondary to nerve compression or involvement of nearby sensory nerves.
Individuals with spinal accessory nerve damage may notice a tingling sensation or numbness in their neck or shoulder area. This can be a result of nerve compression, which affects the transmission of sensory signals. The abnormal sensations can range from a mild tingling to a complete loss of sensation in the affected area. These sensory symptoms can be distressing and may require medical attention to address the underlying cause of the nerve damage.
Motor Function Symptoms
Motor function symptoms are the most common and noticeable manifestations of spinal accessory nerve damage. Affected individuals may struggle to perform simple tasks, such as lifting objects, reaching overhead, or turning their head. Muscle weakness or atrophy may also be observed. It is important to note that the severity of these symptoms will vary depending on the extent of the nerve damage and the specific muscles involved.
Individuals with spinal accessory nerve damage may experience significant muscle weakness in their shoulders, making it difficult to lift objects or perform activities that require upper body strength. The muscles responsible for rotating the head may also be affected, causing limited mobility and discomfort. Over time, muscle atrophy may occur, further impacting the individual’s ability to perform everyday tasks.
Furthermore, the impact of motor function symptoms can extend beyond physical limitations. The frustration and emotional toll of not being able to perform simple movements can lead to decreased self-esteem and a sense of dependency on others for assistance. Rehabilitation and physical therapy may be necessary to regain strength and improve motor function in individuals with spinal accessory nerve damage.
Diagnostic Procedures for Spinal Accessory Nerve Damage
Clinical Examination
A comprehensive clinical examination is often the first step in diagnosing spinal accessory nerve damage. The healthcare provider will carefully assess muscle strength, range of motion, and coordination of the head and neck muscles. They may also inquire about the onset, duration, and progression of symptoms to gain a better understanding of the underlying cause. Additional tests may be ordered based on these findings.
During the clinical examination, the healthcare provider will perform various maneuvers to evaluate the function of the spinal accessory nerve. They may ask the patient to shrug their shoulders, turn their head, or lift their arms to assess the strength and coordination of the affected muscles. Additionally, the provider may palpate the neck and shoulder area to check for any areas of tenderness or swelling that may indicate nerve damage.
Furthermore, the healthcare provider may perform a thorough neurological examination to assess other aspects of nerve function. This may involve testing sensation, reflexes, and coordination in different parts of the body to rule out any additional nerve involvement.
Imaging Techniques
Imaging techniques such as magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide detailed images of the head, neck, and surrounding structures. These tests help identify any structural abnormalities or lesions that may be causing or contributing to the nerve damage. Imaging is particularly useful in cases where trauma, tumors, or anatomical anomalies are suspected.
During an MRI or CT scan, the patient lies on a table that slides into a large, tunnel-like machine. The machine uses a magnetic field and radio waves to create detailed images of the internal structures. These images can help the healthcare provider visualize the spinal accessory nerve, as well as any surrounding tissues or structures that may be affecting its function.
In some cases, a contrast dye may be injected into a vein before the imaging test to enhance the visibility of certain structures or abnormalities. This can provide even more detailed information and aid in the diagnosis of spinal accessory nerve damage.
Electromyography and Nerve Conduction Studies
Electromyography (EMG) and nerve conduction studies (NCS) are specialized tests that can evaluate the electrical activity and conduction of nerves and muscles. These tests can help determine the extent of nerve damage, differentiate between nerve entrapment and other neurological conditions, and guide treatment decisions. EMG involves inserting tiny electrodes into the affected muscles, while NCS measures the speed and strength of electrical signals traveling along the nerves.
During an EMG, the healthcare provider will insert small, needle-like electrodes into the muscles that are suspected to be affected by the spinal accessory nerve damage. The electrodes detect the electrical activity produced by the muscles, which can provide valuable information about the health and function of the nerve-muscle connection.
NCS, on the other hand, involves the placement of surface electrodes on the skin overlying the nerves. These electrodes deliver small electrical impulses to the nerves, and the response is recorded. This test measures the speed and strength of the electrical signals as they travel along the nerves, helping to identify any abnormalities or disruptions in the nerve conduction.
Both EMG and NCS are typically performed together to provide a comprehensive assessment of the spinal accessory nerve function. These tests are safe and minimally invasive, and the discomfort is usually minimal.
Treatment Options for Spinal Accessory Nerve Damage
Conservative Management
In cases of mild or partial spinal accessory nerve damage, conservative management may be initially recommended. This may involve physical therapy, pain management strategies, and lifestyle modifications. Physical therapy exercises can help improve muscle strength, range of motion, and overall functionality. Pain management techniques such as medication, heat or cold therapy, or alternative therapies like acupuncture may be employed to alleviate discomfort and facilitate recovery.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation form a crucial part of the treatment plan for spinal accessory nerve damage. A skilled physical therapist can work with the patient to develop a comprehensive rehabilitation program tailored to their specific needs. This may include exercises to strengthen the affected muscles, improve coordination and balance, and restore functional abilities. The therapist may also incorporate manual techniques, such as massage or joint mobilization, to alleviate pain and enhance recovery.
Surgical Interventions
In cases of severe or complete spinal accessory nerve damage, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause and extent of the nerve damage. Nerve repair or nerve grafting techniques may be utilized to restore nerve function. In certain situations, nerve transfers, where a working nerve is rewired to innervate the affected muscles, can also be employed. It is important to note that surgical interventions carry risks and should only be considered after a thorough evaluation and discussion with a surgical specialist.
Prognosis and Recovery from Spinal Accessory Nerve Damage
Factors Influencing Recovery
The prognosis and recovery outlook for individuals with spinal accessory nerve damage can vary significantly depending on several factors. The extent and location of the nerve damage, the underlying cause, the individual’s overall health, and promptness of intervention all play a role in determining the recovery potential. It is important to approach each case individually and remain optimistic while considering the long-term management and care required.
Potential Complications and Challenges
While many individuals with spinal accessory nerve damage recover well with appropriate treatment and rehabilitation, there can be potential complications and challenges along the way. These may include persistent weakness or muscle atrophy, chronic pain, loss of function, and psychological impacts due to the limitations imposed by the nerve damage. Collaborating closely with healthcare professionals and support networks can help address these challenges and optimize outcomes.
Long-Term Management and Care
Long-term management and care are essential for individuals with spinal accessory nerve damage. This may involve ongoing physical therapy or rehabilitation to maintain muscle strength and functionality. Regular follow-up appointments with healthcare professionals allow monitoring of progress and addressing any emerging concerns. The individual should remain proactive in their own care, adopting healthy lifestyle choices and seeking professional help whenever necessary to ensure the best possible quality of life.
In conclusion, spinal accessory nerve damage can have a significant impact on a person’s ability to carry out daily activities and maintain a good quality of life. Prompt recognition and appropriate management of the symptoms are crucial for optimizing outcomes. If you suspect you may have spinal accessory nerve damage or are experiencing any symptoms mentioned in this article, it is imperative to consult with a qualified healthcare professional. They can provide a thorough evaluation, accurate diagnosis, and guide you through the best course of treatment and rehabilitation tailored to your specific needs.