where does the accessory nerve pass through the cranium
The accessory nerve, also known as the cranial nerve XI, is a vital component of the human nervous system. It plays a crucial role in motor functions, particularly those involving the muscles of the neck, shoulder, and upper back. Understanding the intricate details of this nerve’s anatomy and pathway can shed light on its significance and clinical implications.
Understanding the Accessory Nerve
Definition and Function of the Accessory Nerve
The accessory nerve, also known as cranial nerve XI, is considered one of the twelve cranial nerves that play a crucial role in the functioning of the human body. Unlike other cranial nerves that emerge directly from the brainstem, the accessory nerve has a unique origin. It arises from the ventral horn of the upper spinal cord, specifically from the first five segments of the cervical spinal cord.
Primarily functioning as a motor nerve, the accessory nerve coordinates movements of the sternocleidomastoid muscle and the trapezius muscle. These muscles are essential for proper head and shoulder movements, such as turning the head and shrugging the shoulders. The accessory nerve is responsible for the efficient communication between the brain and these muscles, ensuring smooth and coordinated movements.
Understanding the anatomy and pathway of the accessory nerve is crucial in comprehending its role in the human body.
Anatomy of the Accessory Nerve
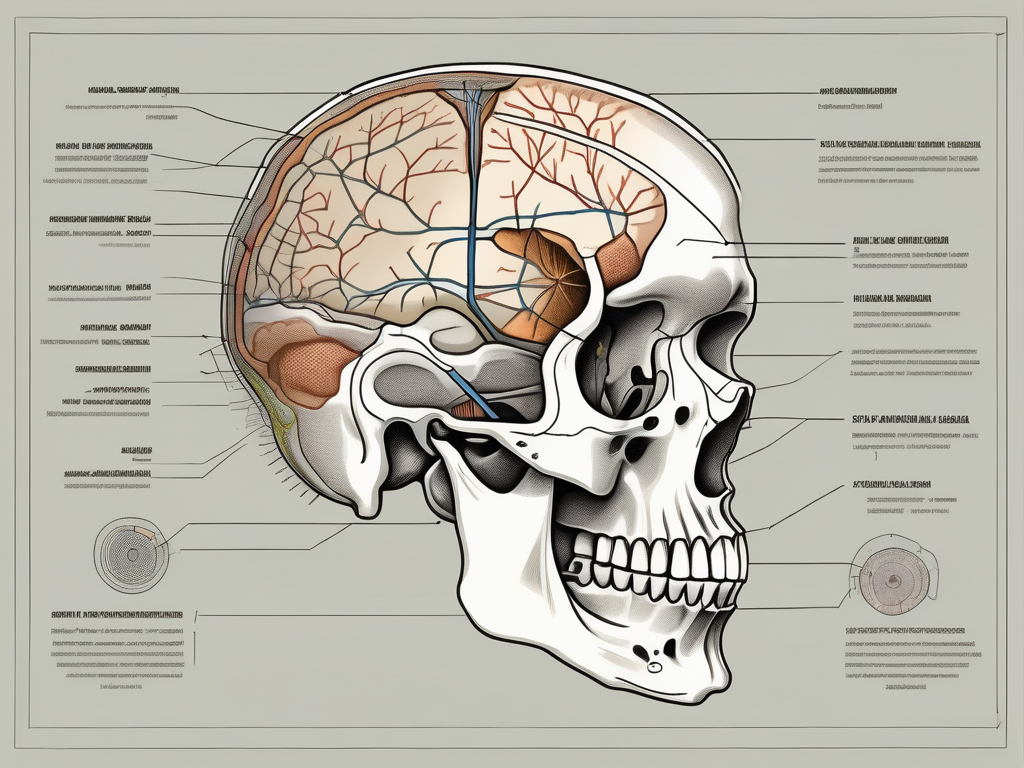
The accessory nerve’s pathway through the cranium involves a fascinating journey. It emerges from the spinal cord through the jugular foramen, which is an opening located on the skull’s base. This foramen is adjacent to the temporal bone and allows the accessory nerve to enter the cranium, bringing it closer to its vital structures.
Once inside the cranium, the accessory nerve travels alongside the internal jugular vein, another significant component found within the jugular foramen. Together, they navigate the complex terrain of the cranial cavity, eventually reaching their respective destinations.
The accessory nerve branches out into two main divisions: the spinal accessory nerve and the cranial accessory nerve. The spinal accessory nerve innervates the sternocleidomastoid muscle, which is responsible for turning the head from side to side, as well as tilting the head forward and backward. The cranial accessory nerve innervates the trapezius muscle, which plays a crucial role in shoulder movements, such as shrugging and rotating the scapula.
It is fascinating to note that the accessory nerve not only controls voluntary movements but also plays a role in regulating the autonomic nervous system. This means that it contributes to the control of involuntary actions, such as heart rate, blood pressure, and digestion.
Understanding the intricate anatomy and function of the accessory nerve provides valuable insights into the complexity of the human nervous system and its role in maintaining optimal bodily functions.
The Pathway of the Accessory Nerve
Origin of the Accessory Nerve
The accessory nerve, also known as cranial nerve XI, originates from the cervical spinal cord. More specifically, it arises from the ventral horn of the upper segments. This unique location sets it apart from the other cranial nerves, as it is partly rooted in the spinal cord.
From its origin, the accessory nerve embarks on a fascinating and intricate journey, carefully navigating the structures within the cranium. This complex pathway allows the nerve to fulfill its essential role in muscular coordination and control.
Route of the Accessory Nerve through the Cranium
After emerging from the cervical spinal cord, the accessory nerve travels superiorly through the foramen magnum. This opening serves as a connection between the spinal cord and the cranium, allowing the nerve to enter the skull.
Once inside the cranium, the accessory nerve gradually follows a specific path, making its way towards its intended destinations. This journey is filled with remarkable anatomical details and interactions.
As the accessory nerve continues its course through the skull, it passes through the jugular foramen. This crucial opening, located at the base of the skull, provides a safe passage for the nerve, shielding it from potential compressive forces that could impede its function.
Entering the jugular foramen, the accessory nerve encounters the internal jugular vein. This major blood vessel arises from the sigmoid sinus, and interestingly, it shares the same tight space with the accessory nerve. This coexistence within such a confined area is an incredible demonstration of anatomical efficiency and adaptation.
As the accessory nerve and the internal jugular vein travel together through the jugular foramen, they continue their separate paths, each fulfilling their unique functions. The accessory nerve proceeds to innervate various muscles, including the sternocleidomastoid and trapezius muscles, contributing to head and shoulder movements.
The intricate pathway of the accessory nerve through the cranium showcases the remarkable complexity and precision of the human anatomy. It is a testament to the intricacies of the nervous and vascular systems, highlighting the harmonious coexistence of structures within the limited space of the skull.
The Accessory Nerve and the Cranial Structures
The accessory nerve, also known as cranial nerve XI, plays a crucial role in the functioning of various cranial structures. One such significant junction is the meeting point of the accessory nerve and the internal jugular vein within the jugular foramen.
Located at the base of the skull, the jugular foramen serves as a gateway for multiple cranial structures, consolidating several key elements within a relatively small area. This intricate network of nerves, veins, and other structures requires careful evaluation during diagnostic procedures to ensure optimal functioning.
Pathologies affecting the jugular foramen can have implications not only for the accessory nerve but also for nearby structures. The close proximity between the accessory nerve, internal jugular vein, and other vital components necessitates a comprehensive understanding of their interconnections.
The Accessory Nerve and the Jugular Foramen
Within the jugular foramen, the accessory nerve and the internal jugular vein form a unique relationship. This convergence of structures highlights the intricate nature of the cranial anatomy.
The accessory nerve, originating from the medulla oblongata and the upper spinal cord, travels through the jugular foramen alongside the internal jugular vein. This coexistence emphasizes the importance of the accessory nerve in the overall functioning of the head and neck region.
Understanding the complex interactions within the jugular foramen is essential for healthcare professionals when diagnosing and treating conditions that may affect the accessory nerve and its associated structures.
The Accessory Nerve and the Sternocleidomastoid Muscle
The accessory nerve’s relationship with the sternocleidomastoid muscle is vital for maintaining optimal head movements and overall functionality of the neck region.
The sternocleidomastoid muscle, a paired muscle located on each side of the neck, plays a significant role in various movements. It acts to flex the neck laterally and rotate the head to the opposite side, allowing for a wide range of motion.
Damage or dysfunction of the accessory nerve can result in weakness or paralysis of the sternocleidomastoid muscle on one side. This can lead to limited range of motion, muscle imbalances, and potential musculoskeletal issues.
Healthcare professionals must carefully assess the relationship between the accessory nerve and the sternocleidomastoid muscle to identify any abnormalities or dysfunctions that may impact the patient’s overall well-being.
Clinical Significance of the Accessory Nerve
The accessory nerve, also known as cranial nerve XI, plays a crucial role in the motor function of the neck and shoulder muscles. It originates in the brainstem and travels down through the skull to innervate the sternocleidomastoid and trapezius muscles.
When the accessory nerve sustains damage or faces dysfunction, individuals may experience various symptoms. These can include weakness, muscle atrophy, and pain in the neck, shoulder, and upper back regions. These symptoms can significantly impact a person’s quality of life and ability to perform daily activities.
Conditions such as nerve entrapment, trauma, tumors, or surgical procedures involving the neck and shoulder region can potentially impact the accessory nerve. Nerve entrapment occurs when the nerve becomes compressed or trapped, leading to impaired function. Trauma, such as a neck injury or whiplash, can cause direct damage to the nerve fibers. Tumors in the vicinity of the accessory nerve can also exert pressure on the nerve, leading to dysfunction. Additionally, surgical procedures in the neck and shoulder region carry a risk of damaging the accessory nerve.
Seeking medical attention and proper diagnosis is crucial in order to determine the underlying cause and implement appropriate treatment strategies. As with any medical concern, consulting with a healthcare professional, such as a neurologist or neurosurgeon, is essential. They can conduct a thorough evaluation and utilize imaging techniques, such as MRI or CT scans, to assess the condition of the accessory nerve and develop a suitable management plan.
Diagnostic Procedures for Accessory Nerve Pathologies
When investigating accessory nerve pathologies, medical professionals often employ a combination of diagnostic techniques to accurately assess the condition. This may include a comprehensive physical examination, medical history review, and imaging studies to assess the integrity of the nerve and associated structures.
During a physical examination, the healthcare professional will assess the strength and range of motion of the neck and shoulder muscles. They may also perform specific tests, such as the shoulder shrug test or the head rotation test, to evaluate the function of the accessory nerve.
In addition to the physical examination, imaging studies are commonly used to visualize the accessory nerve and identify any abnormalities. Magnetic resonance imaging (MRI) and computed tomography (CT) scans can provide detailed images of the nerve and surrounding structures, helping to pinpoint the location and extent of any damage or dysfunction.
Electromyography (EMG) and nerve conduction studies are further diagnostic methods used to evaluate the functionality of the accessory nerve. EMG involves the insertion of small needles into the affected muscles to measure their electrical activity. Nerve conduction studies, on the other hand, assess the speed and strength of the electrical signals transmitted through the accessory nerve.
By combining the findings from these various diagnostic procedures, healthcare professionals can accurately diagnose accessory nerve pathologies and develop an individualized treatment plan. Treatment options may include physical therapy, medication, nerve blocks, or in severe cases, surgical intervention.
Frequently Asked Questions about the Accessory Nerve
Common Misconceptions about the Accessory Nerve
While the anatomy and function of the accessory nerve are foundational to understanding its importance, there are often misconceptions surrounding this nerve. Addressing these misconceptions can help provide accurate and reliable information to individuals seeking to expand their knowledge:
- Does the accessory nerve only control neck movements?
- Can accessory nerve damage be permanent?
- Are accessory nerve pathologies common?
While the accessory nerve indeed plays a significant role in neck movements, its function extends beyond this area. The nerve also contributes to proper shoulder movements, aiding in the control of the trapezius muscle.
Moreover, the accessory nerve is not solely responsible for neck and shoulder movements. It works in conjunction with other nerves and muscles to ensure coordinated and precise motion. This collaboration allows for a wide range of movements, including rotation, flexion, and extension of the neck and shoulder.
The recovery from accessory nerve damage can vary depending on the cause and extent of the injury. In some cases, proper treatment and rehabilitation can lead to a significant improvement in function. However, in severe cases, complete recovery may not be possible, and residual effects may persist.
It is important to note that early intervention and appropriate management play a crucial role in maximizing the chances of recovery. Physical therapy, occupational therapy, and other rehabilitative techniques can aid in restoring functionality and minimizing long-term consequences.
In comparison to other cranial nerve pathologies, accessory nerve-related conditions are relatively uncommon. However, certain factors like trauma, surgery, or tumors in the neck region can increase the likelihood of developing these specific conditions.
It is essential to consult with healthcare professionals if any symptoms or concerns arise. Prompt diagnosis and treatment can help mitigate the impact of accessory nerve pathologies and improve overall outcomes.
Future Research Directions for the Accessory Nerve
The ongoing advancement in medical and scientific research presents exciting opportunities for studying the accessory nerve further. Future investigations may focus on refining diagnostic techniques, exploring potential treatment modalities, and enhancing our understanding of the nerve’s intricate connections within the cranial cavity.
Researchers are actively exploring the potential role of regenerative medicine in restoring damaged accessory nerves. Novel approaches, such as stem cell therapy and tissue engineering, hold promise for promoting nerve regeneration and functional recovery.
Additionally, advancements in neuroimaging techniques, such as magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI), enable researchers to visualize the accessory nerve and its connections with greater clarity. These imaging modalities provide valuable insights into the structural and functional aspects of the nerve, aiding in the development of targeted interventions.
While there is already a vast array of knowledge surrounding the accessory nerve, continued research efforts hold the potential to deepen our understanding and pave the way for novel therapeutic interventions.
In conclusion, the accessory nerve passes through the cranium via the jugular foramen alongside the internal jugular vein. Its intricate pathway allows it to play a crucial role in coordinating movements of the neck and shoulder muscles. Understanding the anatomy, function, and clinical significance of the accessory nerve provides essential knowledge for healthcare professionals and individuals seeking to enhance their understanding of this remarkable neural structure.


