what test would be performed when assessing motor function of the spinal accessory nerve
The spinal accessory nerve, also known as cranial nerve XI, is an important component of the nervous system. It plays a crucial role in the motor function of the neck and shoulders. Assessing the motor function of this nerve is vital in diagnosing and managing various conditions that may affect its normal function.
Understanding the Spinal Accessory Nerve
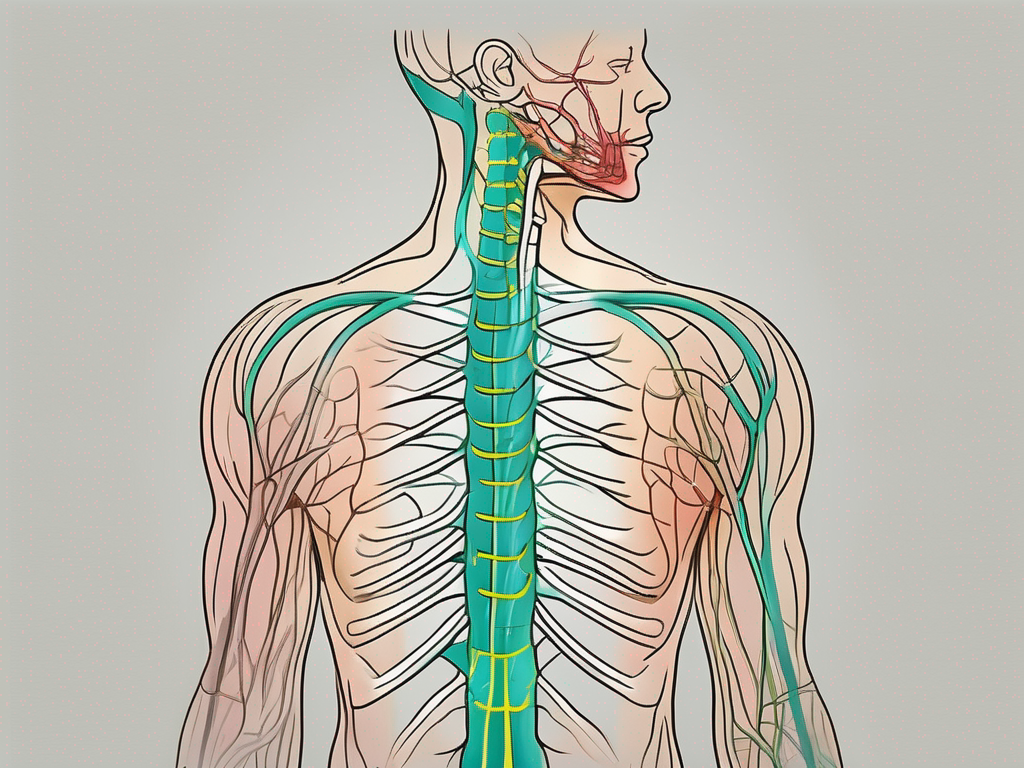
The spinal accessory nerve is a crucial component of the nervous system, playing a vital role in the movement and coordination of the neck and shoulder muscles. It originates in the brainstem and travels down the spinal cord, exiting the skull through the jugular foramen.
Once it emerges from the skull, the spinal accessory nerve branches out to innervate the sternocleidomastoid and trapezius muscles. These muscles are responsible for a wide range of movements, including rotation of the head, flexion and extension of the neck, and elevation and retraction of the shoulders.
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve consists of two roots: the cranial root and the spinal root. The cranial root originates in the brainstem, specifically in the lower part of the medulla oblongata and the upper part of the spinal cord. It then joins the fibers of the spinal root in the upper cervical spinal cord, forming the main trunk of the nerve.
From this main trunk, the spinal accessory nerve extends its branches to innervate the sternocleidomastoid and trapezius muscles. The sternocleidomastoid muscle, located on the sides of the neck, allows us to rotate our head and flex and extend our neck. The trapezius muscle, which covers a large portion of the upper back and neck, enables us to elevate and retract our shoulders.
Role and Function of the Spinal Accessory Nerve
The spinal accessory nerve plays a crucial role in the movement and coordination of the neck and shoulder muscles. It is responsible for enabling us to perform essential activities in our daily lives, such as turning our head to look around, lifting and carrying objects overhead, and maintaining proper posture.
When the spinal accessory nerve is functioning properly, it allows for smooth and coordinated movements of the neck and shoulders. However, any disruption in its motor function can lead to difficulties in performing these movements and result in limitations in daily activities.
Damage or injury to the spinal accessory nerve can occur due to various reasons, including trauma, surgical procedures, or certain medical conditions. When this happens, individuals may experience weakness, pain, or limited range of motion in the affected muscles.
Assessing the motor function of the spinal accessory nerve is an important part of diagnosing and treating any potential issues. Healthcare professionals may use a variety of tests, such as manual muscle testing, to evaluate the strength and function of the sternocleidomastoid and trapezius muscles.
Understanding the anatomy and role of the spinal accessory nerve is essential for healthcare professionals in providing accurate diagnoses and developing appropriate treatment plans. By recognizing the importance of this nerve and its impact on our daily lives, we can appreciate the complexity and intricacy of the human body’s nervous system.
Tests for Assessing Motor Function of the Spinal Accessory Nerve
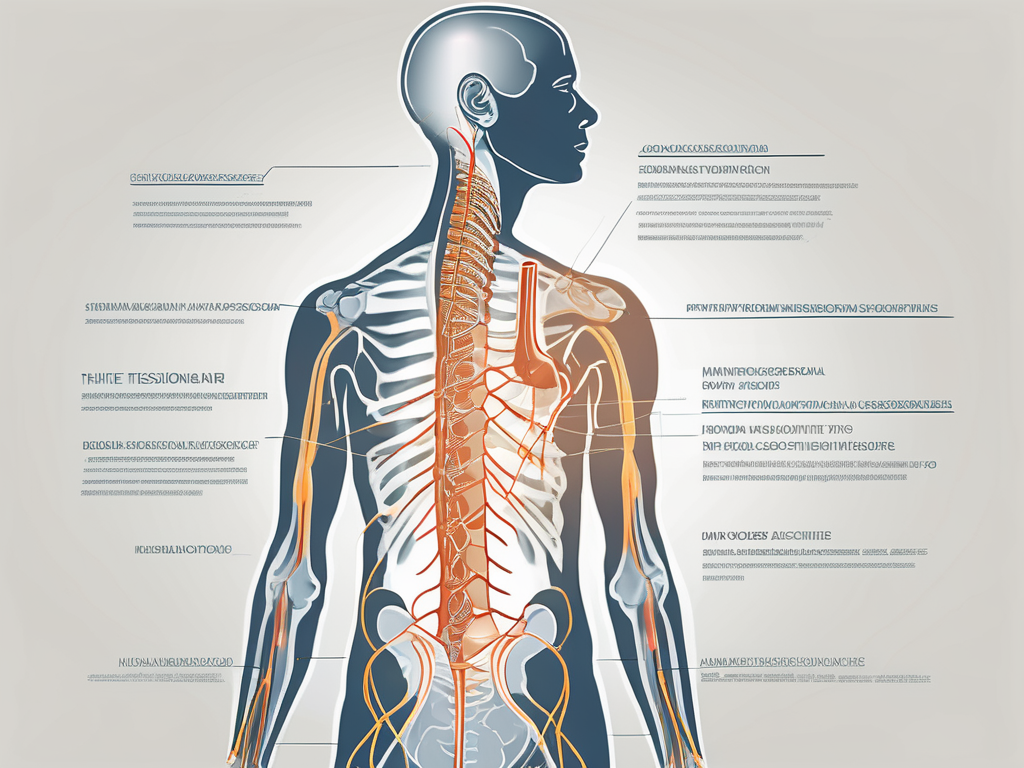
When assessing the motor function of the spinal accessory nerve, healthcare professionals employ a variety of tests. These tests aim to evaluate the strength, coordination, and range of motion of the associated muscles.
The spinal accessory nerve, also known as cranial nerve XI, plays a crucial role in controlling the movement of certain muscles in the neck and shoulders. Dysfunction of this nerve can lead to weakness or paralysis of these muscles, affecting the individual’s ability to perform daily activities.
Physical Examination Techniques
During a physical examination, the healthcare provider may assess the strength and function of the muscles innervated by the spinal accessory nerve. They may ask the patient to perform specific movements, such as shrugging the shoulders or turning the head against resistance. Observing muscle strength, symmetry, and any abnormal patterns of movement can provide important clues about the nerve’s motor function.
In addition, the healthcare provider may check for any tender points or areas of muscle atrophy that could be indicative of nerve dysfunction. These physical examination techniques are usually the initial steps in assessing the motor function of the spinal accessory nerve.
Furthermore, the healthcare provider may also evaluate the patient’s posture and gait, as abnormalities in these areas can be associated with spinal accessory nerve dysfunction. They may observe the patient’s ability to maintain an upright posture and walk without any noticeable abnormalities.
Electromyography and Nerve Conduction Studies
Electromyography (EMG) and nerve conduction studies (NCS) are commonly used to objectively evaluate the function of nerves and muscles. EMG involves inserting small electrodes into the muscles to measure the electrical activity that occurs during muscle contraction and relaxation. NCS, on the other hand, measures the speed and strength of electrical signals as they travel along the nerve.
By performing EMG and NCS, healthcare professionals can determine if there is any damage or dysfunction in the spinal accessory nerve or the muscles it innervates. These tests provide valuable information about the integrity and function of the nerve, helping to guide diagnosis and treatment decisions.
During an EMG, the healthcare provider may ask the patient to perform specific movements while the electrodes are inserted into the muscles. This allows for the assessment of the electrical activity produced by the muscles during these movements.
In NCS, small electrical shocks are applied to the nerve, and the resulting electrical signals are measured. This helps determine the speed and strength of the nerve’s conduction, providing insights into its function.
Imaging Techniques in Nerve Assessment
Imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used in certain cases to assess the structural integrity of the spinal accessory nerve. These imaging modalities can help identify any abnormalities, such as tumors or injury, that may be impacting the nerve’s motor function.
Although imaging techniques alone cannot evaluate the nerve’s motor function, they can provide important information to complement the findings from physical examinations and specialized tests like EMG and NCS.
During an MRI or CT scan, detailed images of the neck and shoulder region are obtained. These images can reveal any structural abnormalities, such as nerve compression or tumors, that may be affecting the spinal accessory nerve. The healthcare provider can then use this information to guide further diagnostic and treatment interventions.
In conclusion, assessing the motor function of the spinal accessory nerve involves a comprehensive approach that includes physical examination techniques, electromyography, nerve conduction studies, and imaging techniques. These tests provide valuable insights into the integrity and function of the nerve, helping healthcare professionals make accurate diagnoses and develop appropriate treatment plans.
Interpreting Test Results
Interpreting the results of tests used to assess the motor function of the spinal accessory nerve requires expertise and experience. The healthcare provider will compare the findings from physical examinations, EMG, NCS, and imaging studies to form a comprehensive assessment of the nerve’s function.
During a physical examination, the healthcare provider will carefully evaluate the patient’s range of motion, muscle strength, and any signs of muscle atrophy or weakness. They will also assess the patient’s ability to perform specific movements that require the involvement of the spinal accessory nerve, such as shrugging the shoulders or turning the head.
In addition to the physical examination, electromyography (EMG) and nerve conduction studies (NCS) are commonly used to evaluate the function of the spinal accessory nerve. EMG involves the insertion of small electrodes into the muscles associated with the nerve. These electrodes detect and record the electrical activity generated by the muscles, providing valuable information about the nerve’s function.
Nerve conduction studies, on the other hand, measure the speed and strength of electrical signals as they travel along the spinal accessory nerve. By stimulating the nerve at one point and recording the response at another, healthcare professionals can assess the integrity of the nerve and identify any abnormalities.
Normal vs Abnormal Findings
Normal findings indicate that the sensory and motor functions of the spinal accessory nerve are intact, and there are no significant abnormalities affecting its function. The physical examination may reveal symmetrical muscle strength and range of motion, while the EMG and NCS results will show normal electrical activity and conduction along the nerve.
On the other hand, abnormal findings may suggest various conditions or injuries that need further investigation and management. In some cases, the physical examination may reveal muscle weakness or atrophy on one side of the body, indicating a potential problem with the spinal accessory nerve. The EMG and NCS results may show reduced electrical activity or slower conduction speeds, indicating a disruption in the nerve’s function.
It’s important to remember that abnormal test results do not automatically equate to a diagnosis. Further evaluation and consultation with a healthcare professional are necessary for accurate interpretation and appropriate management. Additional tests, such as imaging studies like magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be ordered to provide a more detailed view of the nerve and surrounding structures.
Potential Disorders and Conditions
Abnormal test results involving the spinal accessory nerve may be indicative of certain disorders or conditions. These can range from nerve entrapment or injury to tumors affecting the nerve or its associated muscles. Nerve entrapment, such as thoracic outlet syndrome, can compress the spinal accessory nerve and lead to motor dysfunction.
Tumors, both benign and malignant, can also affect the spinal accessory nerve. For example, a tumor in the neck region may put pressure on the nerve, causing weakness or paralysis of the associated muscles. Additionally, conditions such as spinal accessory nerve palsy, Bell’s palsy, or cervical spine disorders may result in motor dysfunction of this nerve.
Consulting with a healthcare professional is crucial for accurate diagnosis, treatment planning, and appropriate management of any identified disorder or condition. Depending on the underlying cause, treatment options may include physical therapy, medication, surgery, or a combination of these approaches.
In conclusion, interpreting test results for the spinal accessory nerve requires a comprehensive evaluation of physical examinations, EMG, NCS, and imaging studies. Normal findings indicate the nerve’s intact function, while abnormal findings may suggest various disorders or conditions that require further investigation and management. Consulting with a healthcare professional is essential for accurate interpretation and appropriate treatment planning.
Treatment Options for Spinal Accessory Nerve Dysfunction
The management of spinal accessory nerve dysfunction depends on the underlying cause and the extent of motor impairment. Treatment options may include non-surgical interventions or, in severe cases, surgical interventions.
Non-Surgical Interventions
Non-surgical interventions often involve conservative approaches aimed at pain relief, reducing inflammation, and improving muscle strength and function. These may include physical therapy, targeted exercises, medication, and other modalities such as heat or cold therapy.
Physical therapy techniques, including stretching, strengthening, and range-of-motion exercises, can help improve muscle function and reduce the risk of further complications. These exercises are designed to specifically target the affected muscles and promote their recovery. Additionally, modifying certain activities or using assistive devices may be beneficial in conservatively managing spinal accessory nerve dysfunction.
Medication can also play a role in managing the symptoms associated with spinal accessory nerve dysfunction. Nonsteroidal anti-inflammatory drugs (NSAIDs) may be prescribed to reduce inflammation and alleviate pain. Muscle relaxants can help relieve muscle spasms, while analgesics can provide pain relief. In some cases, corticosteroid injections may be administered to reduce inflammation and swelling in the affected area.
Other non-surgical modalities, such as heat or cold therapy, may be used to provide symptomatic relief. Heat therapy, in the form of hot packs or warm baths, can help relax muscles and improve blood circulation. Cold therapy, using ice packs or cold compresses, can help reduce inflammation and numb the affected area, providing temporary pain relief.
It’s essential to work closely with a healthcare professional to develop an individualized treatment plan tailored to the specific needs and goals of the patient. Regular follow-up appointments and adjustments to the treatment plan may be necessary to ensure optimal outcomes.
Surgical Interventions
In severe cases where conservative treatments fail to provide satisfactory results, surgical interventions may be considered. The specific surgical approach depends on the underlying cause of spinal accessory nerve dysfunction and may involve nerve decompression, repair, or reconstruction.
Nerve decompression surgery aims to relieve pressure on the affected nerve by removing any structures or tissues that may be compressing it. This can help restore normal nerve function and alleviate symptoms such as muscle weakness or pain. Repair or reconstruction surgeries may be performed to address any damage or injury to the spinal accessory nerve, restoring its integrity and function.
Surgical interventions require careful evaluation and discussion with a specialist, as they carry their own risks and potential complications. The decision to undergo surgery should be made in collaboration with a neurosurgeon or a specialized healthcare provider who can provide expert guidance. They will thoroughly assess the patient’s condition, discuss the benefits and risks of surgery, and explore alternative treatment options if appropriate.
Post-surgical rehabilitation is an essential part of the recovery process. Physical therapy and rehabilitation exercises are typically prescribed to help regain muscle strength, improve range of motion, and optimize functional outcomes. The rehabilitation program will be tailored to the individual needs of the patient and may involve a combination of exercises, manual therapy techniques, and assistive devices to aid in the recovery process.
Overall, the treatment of spinal accessory nerve dysfunction requires a comprehensive and multidisciplinary approach. The goal is to alleviate symptoms, improve motor function, and enhance the quality of life for individuals affected by this condition. Through a combination of non-surgical interventions and, when necessary, surgical interventions, healthcare professionals strive to provide the most effective and personalized treatment options for each patient.
Rehabilitation and Recovery
Rehabilitation is a vital component of the management of spinal accessory nerve dysfunction. Recovering from this condition often requires a comprehensive and individualized approach that includes physical therapy and long-term management strategies.
Physical Therapy Techniques
Physical therapy plays a significant role in restoring muscle strength, flexibility, and coordination after spinal accessory nerve dysfunction. A physical therapist can design a personalized rehabilitation program that includes targeted exercises, stretching, and manual techniques to promote functional recovery.
Rehabilitation may also involve modalities such as heat or cold therapy, ultrasound, or electrical stimulation to aid in pain relief and enhance tissue healing.
Long-Term Management and Prognosis
The prognosis of spinal accessory nerve dysfunction varies depending on the underlying cause and the extent of nerve damage. The recovery process can be gradual and may require long-term management to optimize the return of motor function.
Long-term management may include regular follow-up appointments, continued physical therapy, self-care practices, and lifestyle modifications. It is crucial to maintain open communication with healthcare professionals and adhere to their recommendations to achieve the best possible outcome.
In conclusion, assessing the motor function of the spinal accessory nerve involves a combination of physical examinations, specialized tests, and imaging techniques. The interpretation of the test results requires expertise and experience to accurately diagnose and manage potential disorders or conditions affecting this important nerve. Treatment options may include non-surgical interventions and, in severe cases, surgical interventions. Rehabilitation and long-term management are crucial aspects of the recovery process. If you are experiencing any symptoms or concerns related to the motor function of the spinal accessory nerve, it is advisable to consult with a healthcare professional for appropriate evaluation, diagnosis, and treatment.