what is a symptom of damage to the spinal accessory nerve
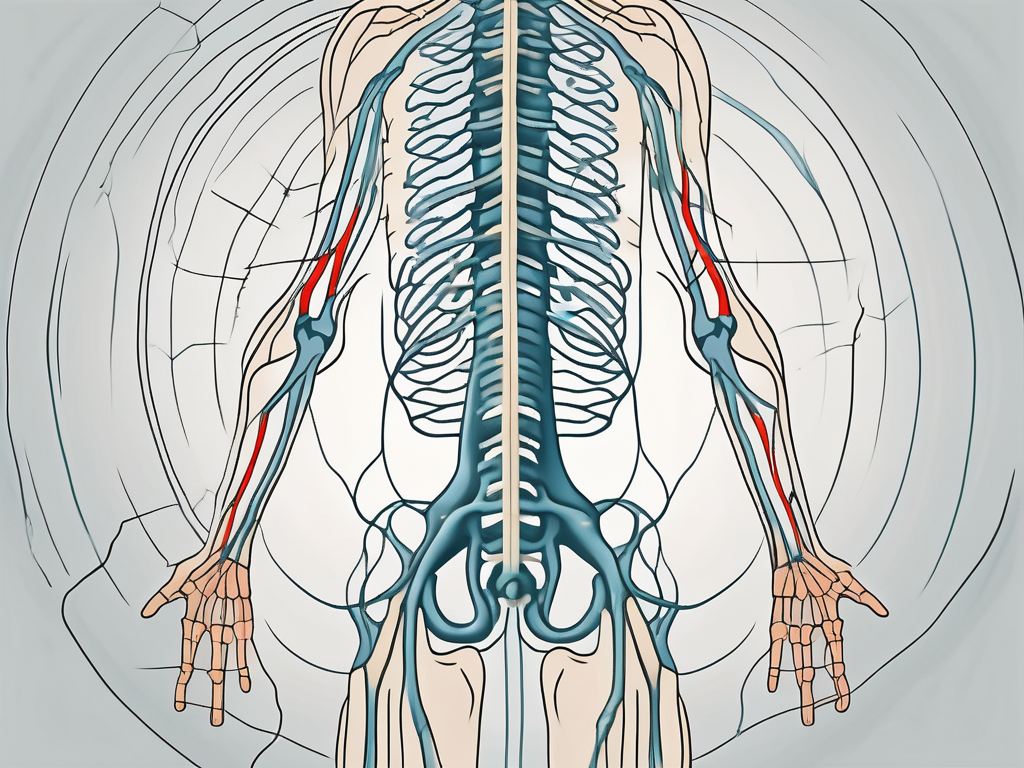
The spinal accessory nerve, also known as cranial nerve XI, is an important nerve that plays a crucial role in the movement and function of certain muscles in the neck and shoulder region. Damage to this nerve can lead to various symptoms and impairments, affecting an individual’s daily activities and quality of life. In this article, we will explore the anatomy and function of the spinal accessory nerve, discuss the causes of nerve damage, identify the symptoms associated with its impairment, explore diagnostic procedures for evaluation, examine treatment options, and provide insights into the prognosis and recovery.
Understanding the Spinal Accessory Nerve
The spinal accessory nerve is a crucial component of the nervous system, playing a vital role in enabling various movements of the head, neck, and shoulders. To fully comprehend the significance of this nerve, it is essential to explore its anatomy and function in detail.
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve originates from the motor nuclei in the upper spinal cord, embarking on a complex journey through the brainstem and neck region. Comprised of two distinct parts, the nerve exhibits a cranial part that arises from the brainstem and a spinal part that emerges from the upper spinal cord segments.
The cranial part of the spinal accessory nerve provides motor innervation to the muscles responsible for head and neck movement. Among these muscles are the sternocleidomastoid and trapezius muscles, which play pivotal roles in various actions.
The sternocleidomastoid muscle, innervated by the cranial part of the nerve, facilitates rotation and flexion of the head. This muscle, located on each side of the neck, allows for essential movements such as turning the head to the side and tilting it forward or backward.
The trapezius muscle, on the other hand, is innervated by the spinal part of the spinal accessory nerve. This muscle, which spans the upper back and neck, is responsible for controlling shoulder movements. It aids in scapular stabilization and elevation, allowing for proper posture and a wide range of arm motions.
Function of the Spinal Accessory Nerve
The primary function of the spinal accessory nerve is to coordinate the actions of the sternocleidomastoid and trapezius muscles, enabling precise movements of the head, neck, and shoulders.
Through its innervation of the sternocleidomastoid muscle, the spinal accessory nerve facilitates rotation and flexion of the head. This is particularly important in everyday activities such as looking over one’s shoulder while driving or turning the head to engage in conversation.
Moreover, the trapezius muscle, under the control of the spinal part of the spinal accessory nerve, plays a crucial role in shoulder movements. It aids in scapular stabilization, ensuring the proper alignment and functioning of the shoulder joint. Additionally, the trapezius muscle allows for shoulder elevation, enabling actions such as lifting objects overhead or shrugging the shoulders.
Overall, the spinal accessory nerve’s coordination of the sternocleidomastoid and trapezius muscles contributes to maintaining proper posture, facilitating head rotation, and enabling a wide range of shoulder movements. Without the proper functioning of this nerve, these essential actions would be compromised, significantly impacting everyday activities and quality of life.
Causes of Spinal Accessory Nerve Damage
The spinal accessory nerve, also known as cranial nerve XI, plays a crucial role in controlling the movement of certain muscles in the neck and shoulder region. Damage to this nerve can result in various degrees of impairment, depending on the cause and severity of the injury.
Trauma and Injury
Traumatic events can be a major cause of spinal accessory nerve damage. Motor vehicle accidents, falls, sports injuries, or direct traumas to the neck and shoulder region can all lead to nerve injury. The extent of nerve involvement and the severity of the injury can vary, resulting in different levels of impairment.
Injuries to the spinal accessory nerve can occur through various mechanisms, including nerve stretching, compression, lacerations, or even complete nerve transection. The site and severity of the injury play a significant role in determining the potential for nerve recovery and the prognosis for function restoration.
Rehabilitation and physical therapy are often necessary to help patients regain muscle control and function after spinal accessory nerve damage caused by trauma. These interventions aim to strengthen the remaining nerve pathways and promote neuroplasticity.
Surgical Complications
Surgeries involving the head, neck, or shoulder area can inadvertently damage the spinal accessory nerve. Procedures such as lymph node dissection, neck dissection, or surgeries addressing tumors in these regions may pose a risk to the nerve due to its proximity to the surgical site.
Despite meticulous surgical techniques, nerve injury can occur. Surgeons must ensure appropriate counseling and precautionary measures to minimize the risk of spinal accessory nerve damage in patients undergoing surgical interventions in these areas.
Post-surgical rehabilitation and physical therapy are often crucial in helping patients recover from spinal accessory nerve damage caused by surgical complications. These interventions focus on restoring muscle function and promoting healing in the affected area.
Neurological Disorders
While not directly targeting the spinal accessory nerve, certain neurological conditions can indirectly affect its function. Nerve compression syndromes, infections, or autoimmune disorders can disrupt the normal functioning of nerves in the neck and shoulder region, including the spinal accessory nerve.
Conditions like cervical radiculopathy, brachial plexus injury, or Guillain-Barré syndrome may lead to secondary nerve dysfunction, affecting the spinal accessory nerve and causing symptoms of impairment.
Diagnosing and managing these neurological disorders require a comprehensive approach, involving medical specialists such as neurologists, physical therapists, and rehabilitation experts. Treatment plans often include a combination of medication, physical therapy, and lifestyle modifications to alleviate symptoms and promote nerve healing.
Understanding the causes of spinal accessory nerve damage is crucial in preventing and managing this condition. Whether it is trauma, surgical complications, or underlying neurological disorders, early diagnosis and appropriate treatment can significantly improve the prognosis and quality of life for individuals affected by spinal accessory nerve damage.
Identifying Symptoms of Spinal Accessory Nerve Damage
The spinal accessory nerve plays a crucial role in the movement and coordination of the head, neck, and shoulder muscles. When this nerve is damaged, it can result in a range of physical and neurological symptoms that can significantly impact a person’s daily life.
Physical Symptoms
Damage to the spinal accessory nerve can lead to various physical symptoms that affect the head, neck, and shoulder region. One of the primary physical symptoms is muscle weakness or loss of coordination in the affected muscles. This can make it challenging for individuals to move their head or shoulders freely, leading to a decreased range of motion.
In addition to muscle weakness, patients may also experience pain and stiffness in the neck and shoulder area. The damaged nerve can cause discomfort and limit the ability to perform certain movements. Muscle atrophy, the wasting away of muscle tissue, is another physical symptom that can occur due to spinal accessory nerve damage.
Furthermore, individuals with this condition may notice asymmetry in the neck muscles. The affected side may appear different from the unaffected side, leading to an imbalance in muscle tone. Additionally, the ability to shrug the shoulders effectively may be compromised, making it difficult to perform simple tasks like lifting objects or reaching overhead.
Neurological Symptoms
While physical symptoms are more common, damage to the spinal accessory nerve can also result in neurological symptoms, although these are less frequent. Neurological symptoms may include altered sensation or abnormal reflexes in the affected area. These sensations can range from tingling or numbness to hypersensitivity or a loss of sensation altogether.
It is important to note that the primary manifestation of spinal accessory nerve damage primarily pertains to motor function impairment. This means that the ability to control and coordinate muscle movements is significantly affected, leading to difficulties in performing everyday tasks.
Overall, identifying the symptoms of spinal accessory nerve damage is crucial for early detection and appropriate treatment. If you suspect any issues with your head, neck, or shoulder movements, it is essential to consult a healthcare professional for a thorough evaluation and diagnosis.
Diagnostic Procedures for Spinal Accessory Nerve Damage
Medical History and Physical Examination
Diagnosing spinal accessory nerve damage begins with a thorough medical history assessment and physical examination. The healthcare provider will evaluate the patient’s symptoms, inquire about any traumatic events or surgeries, and assess the range of motion and strength of the affected muscles.
During the physical examination, specific tests, such as shoulder shrug test or resisted head rotation, may be performed to assess the functioning of the spinal accessory nerve and its associated muscles.
Additionally, the healthcare provider will carefully observe the patient’s posture and gait, looking for any abnormalities that may indicate nerve damage. They will also assess the patient’s sensation in the affected area, checking for any numbness or tingling sensations.
Furthermore, the healthcare provider may ask the patient to perform certain movements or exercises to evaluate the coordination and control of the affected muscles. This can help determine the extent of the nerve damage and the impact it has on the patient’s motor function.
Imaging Tests
In cases where the clinical examination raises suspicion of nerve damage, imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be recommended. These tests help visualize the bones, soft tissues, and nerves in the head, neck, and shoulder region, identifying any structural abnormalities or signs of nerve compression.
During an MRI, a strong magnetic field and radio waves are used to create detailed images of the internal structures. This can provide valuable information about the condition of the spinal accessory nerve and its surrounding tissues.
Alternatively, a CT scan uses a series of X-ray images taken from different angles to create cross-sectional images. This can help identify any bony abnormalities or tumors that may be causing the nerve damage.
These imaging tests are non-invasive and painless, allowing healthcare providers to get a closer look at the affected area without the need for surgery.
Electromyography and Nerve Conduction Studies
To further evaluate the function of the spinal accessory nerve and distinguish it from other potential nerve impairments, electromyography (EMG) and nerve conduction studies (NCS) may be performed. These tests involve measuring electrical activity in the muscles and nerve conduction speed, providing valuable information about the integrity and functioning of the nerve.
During an EMG, small electrodes are inserted into the affected muscles to record their electrical activity at rest and during contraction. This can help determine if there is any muscle damage or if the nerve signals are being properly transmitted.
NCS, on the other hand, involves the placement of electrodes on the skin along the path of the spinal accessory nerve. Small electrical pulses are then applied to stimulate the nerve, and the response is recorded. This test can measure the speed at which the nerve signals travel, helping to identify any areas of nerve damage or compression.
By combining the results of the EMG and NCS, healthcare providers can gain a better understanding of the extent and location of the spinal accessory nerve damage, aiding in the development of an appropriate treatment plan.
Treatment Options for Spinal Accessory Nerve Damage
Non-Surgical Treatments
In cases of mild to moderate spinal accessory nerve damage, non-surgical approaches may be employed to manage symptoms and promote functional recovery. Physical therapy plays a crucial role in rehabilitation, focusing on exercises to strengthen the muscles, enhance range of motion, and improve overall motor control in the affected region.
Pain management techniques, such as medications, heat or cold therapy, and transcutaneous electrical nerve stimulation (TENS) may be used to alleviate discomfort. Assistive devices or modifications to the patient’s environment may also be recommended to enhance daily activities and improve quality of life.
Physical therapy sessions typically involve a variety of exercises tailored to the individual’s specific needs. These exercises may include stretching and strengthening exercises for the neck and shoulder muscles, as well as coordination and balance exercises to improve overall motor control. The physical therapist will closely monitor the patient’s progress and make adjustments to the treatment plan as needed.
In addition to physical therapy, other non-surgical treatments may be utilized to aid in the recovery process. These may include acupuncture, massage therapy, and chiropractic care. These alternative therapies can help reduce pain, improve circulation, and promote healing in the affected area.
Surgical Interventions
In severe cases of spinal accessory nerve damage, surgical interventions may be considered as a treatment option. Surgery aims to repair or restore the nerve function, primarily through nerve grafts or nerve transfers. These techniques involve replacing or rerouting nerves from unaffected regions to bridge the gap caused by the nerve injury.
Before undergoing surgery, a thorough evaluation is conducted to assess the extent of the nerve damage and determine the most appropriate surgical approach. This evaluation may include imaging tests, such as MRI or CT scans, to visualize the affected area and identify any potential obstacles or complications.
The surgical procedure itself is performed by a skilled surgeon with expertise in nerve repair. During the surgery, the damaged nerve is carefully identified and repaired using specialized techniques. Nerve grafts involve taking a healthy nerve from another part of the body and using it to bridge the gap in the damaged nerve. Nerve transfers involve rerouting a nearby healthy nerve to restore function to the affected area.
Following surgery, a comprehensive rehabilitation program is essential to optimize recovery and regain function. Physical therapy is a key component of this program, focusing on strengthening the repaired nerve and surrounding muscles, as well as improving coordination and range of motion.
Rehabilitation and Physical Therapy
Following surgery or during conservative management, rehabilitation and physical therapy remain crucial for optimizing recovery and restoring function. Physical therapists work closely with patients to design individualized treatment plans, incorporating exercises, manual therapy techniques, and functional training to improve overall strength, coordination, and range of motion.
Rehabilitation efforts focus on promoting nerve regeneration, preventing muscle contractures, and enhancing functional independence, enabling patients to regain as much function as possible.
Physical therapy sessions may include a combination of passive and active exercises. Passive exercises, such as gentle stretching and range of motion exercises, are initially performed by the physical therapist to help maintain joint mobility and prevent stiffness. As the patient progresses, active exercises, which involve the patient actively moving and using the affected muscles, are introduced to promote strength and coordination.
In addition to exercises, physical therapists may use manual therapy techniques, such as soft tissue mobilization and joint mobilization, to improve tissue flexibility and joint function. These techniques can help reduce pain, increase blood flow, and promote healing in the affected area.
Overall, rehabilitation and physical therapy play a vital role in the treatment of spinal accessory nerve damage, whether through non-surgical or surgical approaches. By addressing the underlying causes of the nerve damage and focusing on restoring function, patients can experience improved quality of life and regain independence in their daily activities.
Prognosis and Recovery from Spinal Accessory Nerve Damage
Factors Influencing Recovery
The prognosis for recovery from spinal accessory nerve damage varies depending on several factors. The severity and site of the nerve injury, the patient’s overall health, and the time between injury and intervention all play crucial roles in determining the potential for nerve regeneration and functional restoration.
Early diagnosis, timely interventions, and adherence to rehabilitation programs significantly contribute to better outcomes and improved recovery.
Potential Complications and Challenges
While many patients with spinal accessory nerve damage experience significant improvement and functional recovery, some individuals may encounter challenges or complications. These may range from persistent muscle weakness or motor limitations to chronic pain or emotional distress related to functional impairments.
It is essential for individuals and their healthcare providers to have open and ongoing communication to address potential complications, manage expectations, and provide appropriate support throughout the recovery process.
Coping and Living with Spinal Accessory Nerve Damage
Living with spinal accessory nerve damage can be challenging, both physically and emotionally. Patients may need to adapt their lifestyle and daily routines to accommodate limitations and manage residual symptoms. Open communication with healthcare professionals, family support, and participation in support groups can provide valuable resources and strategies for coping.
It is crucial for individuals to seek appropriate medical advice, follow recommended treatment plans, and actively engage in rehabilitation efforts to maximize recovery and improve long-term quality of life.
In conclusion, damage to the spinal accessory nerve can result in various symptoms and functional impairments affecting the head, neck, and shoulder region. Understanding the anatomy and function of the nerve, recognizing potential causes of nerve damage, identifying associated symptoms, and implementing appropriate diagnostic procedures all play critical roles in the management of this condition. With early diagnosis, timely interventions, and comprehensive rehabilitation, individuals can achieve optimal recovery and regain functional independence. It is essential to consult with a healthcare professional specializing in nerve injuries to receive appropriate medical advice, guidance, and personalized treatment plans.


