what happens if the spinal accessory nerve is damaged
The spinal accessory nerve is a crucial component of the nervous system, responsible for controlling certain movements of the head, neck, and shoulders. When this nerve sustains damage, it can have significant consequences on a person’s daily life. Understanding the intricacies of the spinal accessory nerve, the causes of damage, symptoms, diagnosis, treatment options, recovery, and prevention is essential for anyone seeking information on this topic.
Understanding the Spinal Accessory Nerve
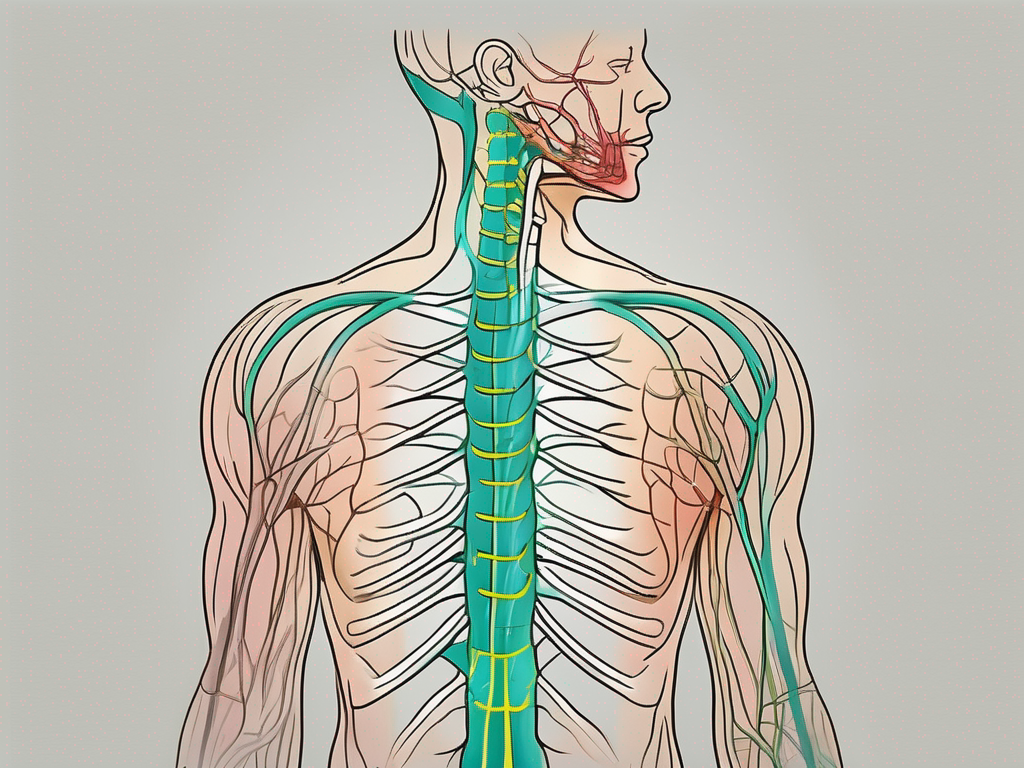
The spinal accessory nerve, also known as cranial nerve XI, is a motor nerve that originates in the brainstem, specifically from the upper cervical spinal cord segments. It then descends down the spinal column and branches out to innervate several key muscles involved in head and neck movement. The nerves mainly control the trapezius and sternocleidomastoid muscles, which play an essential role in shoulder rotation and head turning, respectively.
Let’s delve deeper into the fascinating anatomy and function of the spinal accessory nerve.
Anatomy of the Spinal Accessory Nerve
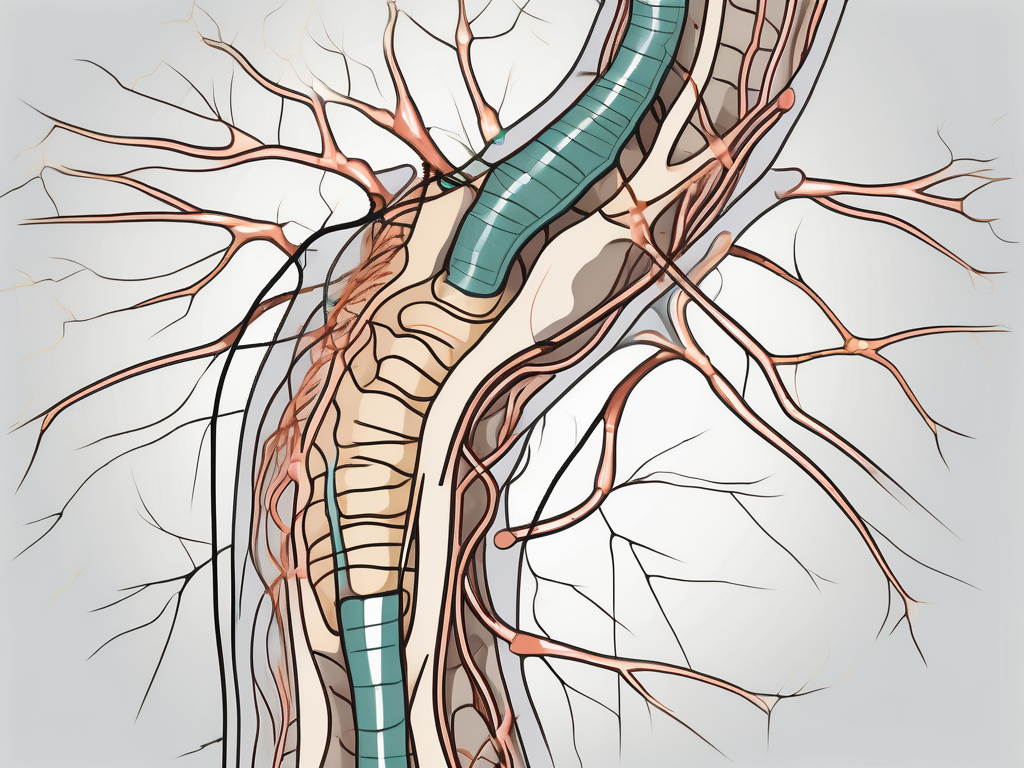
The spinal accessory nerve consists of two main branches: the spinal part and cranial part. The spinal branch arises from the anterior horn motor neurons in the upper cervical spinal cord and merges with the cranial part. This merging occurs within the skull, specifically through the jugular foramen, a bony canal located at the base of the skull.
Once the spinal accessory nerve exits the skull through the jugular foramen, it distributes nerve fibers to numerous muscles in the neck and shoulder region. These muscles include the trapezius, which is responsible for movements such as shrugging the shoulders and retracting the scapulae, and the sternocleidomastoid, which aids in head rotation and flexion.
The intricate network of nerve fibers within the spinal accessory nerve allows for precise control and coordination of these vital muscles.
Function of the Spinal Accessory Nerve
The spinal accessory nerve plays a crucial role in various movements involved in our daily activities. One of its primary functions is to facilitate head rotation, allowing us to turn our heads from side to side. This movement is essential for activities such as checking blind spots while driving or looking over our shoulders.
In addition to head rotation, the spinal accessory nerve also controls shoulder shrugging. When we lift our shoulders towards our ears, it is the trapezius muscle that contracts, thanks to the innervation provided by the spinal accessory nerve. This movement is often used to express confusion, indifference, or uncertainty.
Furthermore, the spinal accessory nerve contributes to lifting the arms above the head. This action is crucial in various sports, such as basketball or volleyball, where players frequently reach above their heads to catch or hit a ball. The nerve’s involvement in this movement ensures proper coordination and stability of the scapulae, allowing for efficient arm movements.
Overall, the spinal accessory nerve’s function extends beyond mere movement. It helps stabilize the scapulae, facilitating proper posture and upper body coordination. Without the spinal accessory nerve, our ability to perform everyday tasks that involve head and shoulder movements would be significantly impaired.
Causes of Spinal Accessory Nerve Damage
Spinal accessory nerve damage can occur due to various factors, including trauma and injury, surgical complications, and specific neurological disorders. Understanding these causes can help in prevention, early detection, and appropriate treatment of this condition.
Trauma and Injury
Accidents or sports-related injuries that cause direct trauma to the neck or shoulder area can result in spinal accessory nerve damage. Motor vehicle collisions, falls, and sports impacts are common causes. The forceful impact on these delicate nerves can disrupt their normal functioning, leading to pain, weakness, and limited mobility. It is important to seek immediate medical attention if you suspect any nerve damage following an injury. Prompt diagnosis and treatment can significantly improve the chances of recovery.
In some cases, the damage may be temporary, and with proper rehabilitation and physical therapy, the nerve function can be restored. However, severe injuries may cause long-term or permanent damage, requiring ongoing management and support.
Surgical Complications
Surgical procedures involving the neck, head, or shoulder region can sometimes lead to inadvertent damage to the spinal accessory nerve. This can occur during lymph node removal, neck dissection surgeries, or other operations in the area. Surgeons take precautions to minimize the risk, such as using nerve monitoring techniques and employing meticulous surgical techniques. However, despite these precautions, nerve damage can still occur.
Symptoms of nerve damage after surgery may include pain, weakness, and difficulty moving the affected muscles. Rehabilitation and physical therapy are often recommended to aid in nerve regeneration and restore function. In some cases, additional surgical interventions may be required to repair or reconstruct the damaged nerve.
Neurological Disorders
Certain neurological disorders, such as amyotrophic lateral sclerosis (ALS) or cervical spinal stenosis, can impair the function of the spinal accessory nerve. ALS is a progressive neurodegenerative disease that affects the nerves and muscles in various parts of the body, including the neck and shoulders. Over time, the nerve cells degenerate, leading to muscle weakness and loss of coordination.
Cervical spinal stenosis, on the other hand, is a condition characterized by the narrowing of the spinal canal in the neck region. This narrowing can put pressure on the spinal accessory nerve, leading to pain, weakness, and limited mobility. Treatment for these neurological disorders focuses on managing symptoms, slowing disease progression, and improving quality of life.
It is important to note that spinal accessory nerve damage can have a significant impact on daily activities, such as lifting objects, reaching overhead, and turning the head. Physical therapy, occupational therapy, and other rehabilitative measures can play a crucial role in helping individuals regain strength, mobility, and independence.
In conclusion, spinal accessory nerve damage can occur due to various causes, including trauma and injury, surgical complications, and specific neurological disorders. Understanding these causes and seeking timely medical attention can help in the diagnosis, treatment, and management of this condition, ultimately improving the overall quality of life for individuals affected by spinal accessory nerve damage.
Symptoms of Spinal Accessory Nerve Damage
Spinal accessory nerve damage can manifest in a variety of symptoms that may significantly impact a person’s daily life. It is important to understand the physical and neurological symptoms that can arise from this condition.
Physical Symptoms
Physical symptoms can include weakness or paralysis in the shoulder and neck muscles. This can result in difficulties with raising the arm, rotating the head, and maintaining proper posture. The affected individual may find it challenging to perform simple tasks such as brushing their hair or lifting objects. The loss of muscle function can lead to a noticeable decrease in strength and endurance.
In addition to weakness, decreased muscle tone and muscle wasting may also be observed. The affected muscles may appear smaller and less defined due to the lack of nerve stimulation. This can further contribute to difficulties in performing everyday activities and may lead to a decrease in overall physical fitness.
Neurological Symptoms
Individuals with spinal accessory nerve damage may experience tingling, numbness, or a loss of sensation in the affected areas. These sensations can be intermittent or constant, depending on the severity of the nerve damage. The tingling or numbness may extend from the neck down to the shoulder and upper back, causing discomfort and affecting the individual’s sense of touch.
In addition to sensory changes, those with spinal accessory nerve damage may also have difficulties with coordination and muscle control. The nerve damage can disrupt the signals sent from the brain to the muscles, leading to uncoordinated movements and a lack of precision. This can make tasks that require fine motor skills, such as writing or buttoning a shirt, challenging and frustrating.
Furthermore, the loss of muscle control can affect the individual’s ability to maintain balance and stability. This can increase the risk of falls and accidents, further impacting their quality of life.
It is important to note that the severity and specific symptoms of spinal accessory nerve damage can vary from person to person. Some individuals may experience only mild symptoms, while others may have more pronounced impairments. Proper diagnosis and treatment are crucial in managing the symptoms and improving the individual’s overall well-being.
Diagnosing Spinal Accessory Nerve Damage
Diagnosing spinal accessory nerve damage typically involves a comprehensive evaluation to assess symptoms, medical history, and additional diagnostic tests.
The evaluation process begins with a thorough review of the patient’s medical history. The doctor will inquire about any previous injuries or medical conditions that may have contributed to the nerve damage. They will also ask about the onset and progression of symptoms, such as weakness or difficulty moving certain muscles.
After gathering the necessary information from the medical history, the doctor will proceed with a physical examination. This examination is crucial in assessing the extent of nerve damage and identifying any associated symptoms or risk factors. The doctor will carefully evaluate muscle strength and coordination, paying close attention to any abnormalities or limitations.
Medical History and Physical Examination
A doctor will review the patient’s medical history and perform a thorough physical examination. They will assess muscle strength and coordination, as well as evaluate any associated symptoms or risk factors.
During the physical examination, the doctor may perform specific tests to assess the function of the spinal accessory nerve. For example, they may ask the patient to perform certain movements, such as shrugging the shoulders or turning the head, to evaluate the nerve’s ability to control these actions. Any weakness or difficulty in performing these movements may indicate damage to the spinal accessory nerve.
Imaging and Laboratory Tests
In some cases, additional diagnostic tests may be necessary to visualize or assess the extent of nerve damage. One common imaging test used is magnetic resonance imaging (MRI). This non-invasive procedure provides detailed images of the structures within the body, allowing the doctor to identify any abnormalities or injuries affecting the spinal accessory nerve.
Nerve conduction studies are another diagnostic tool that may be utilized. This test measures the speed and strength of electrical signals as they travel along the nerves. By analyzing the results, the doctor can determine if there is any disruption or damage to the spinal accessory nerve.
Furthermore, blood tests can be helpful in ruling out other potential causes of nerve dysfunction. Certain medical conditions, such as autoimmune disorders or vitamin deficiencies, can mimic the symptoms of spinal accessory nerve damage. Blood tests can help identify or rule out these underlying conditions, ensuring an accurate diagnosis.
Overall, diagnosing spinal accessory nerve damage requires a comprehensive approach that combines medical history, physical examination, and additional diagnostic tests. By gathering all relevant information, healthcare professionals can accurately assess the extent of the nerve damage and develop an appropriate treatment plan.
Treatment Options for Spinal Accessory Nerve Damage
The treatment of spinal accessory nerve damage depends on the severity and underlying cause of the condition. Spinal accessory nerve damage can occur due to various reasons, such as trauma, surgical complications, or underlying medical conditions.
When it comes to treating spinal accessory nerve damage, healthcare professionals consider both non-surgical and surgical interventions. The choice of treatment depends on the individual’s specific condition and the extent of nerve damage.
Non-Surgical Treatments
Non-surgical interventions play a crucial role in the management of spinal accessory nerve damage. These treatments aim to improve muscle strength, flexibility, and overall function. Physical therapy is often recommended as a primary non-surgical treatment option. During physical therapy sessions, patients undergo exercises and techniques that target the affected muscles and help restore their function.
In addition to physical therapy, occupational therapy may also be beneficial for individuals with spinal accessory nerve damage. Occupational therapists work with patients to develop strategies and techniques that help them perform daily activities more efficiently. They focus on improving fine motor skills, coordination, and functional independence.
Assistive devices, such as braces or splints, may be prescribed to support weakened muscles and enhance stability. These devices can provide additional support and help patients regain their ability to perform certain movements or tasks.
Pain management techniques are also an essential aspect of non-surgical treatment for spinal accessory nerve damage. Medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants, may be prescribed to alleviate discomfort and reduce inflammation. In some cases, therapeutic injections, such as corticosteroids or local anesthetics, may be administered to target specific areas of pain or inflammation.
Surgical Interventions
In certain cases, surgical intervention may be necessary to address spinal accessory nerve damage. Surgery is typically considered when conservative treatments do not yield significant improvements or when the nerve damage is severe.
There are various surgical procedures that can be performed to restore function and alleviate symptoms associated with spinal accessory nerve damage. Nerve repair procedures involve reconnecting the damaged nerve ends to promote nerve regeneration. Surgeons carefully suture the nerve ends together, allowing them to heal and potentially regain their function over time.
In cases where the spinal accessory nerve is severely damaged or irreparable, nerve transfer procedures may be considered. During nerve transfer surgery, a healthy nerve from another part of the body is detached and connected to the damaged spinal accessory nerve. This allows for the transfer of signals and restores muscle function.
It is important to note that the decision to undergo surgery for spinal accessory nerve damage should be made in consultation with a qualified healthcare professional. They will thoroughly evaluate the individual’s condition, discuss the potential risks and benefits of surgery, and determine the most appropriate treatment option.
In conclusion, the treatment options for spinal accessory nerve damage are diverse and depend on the severity and underlying cause of the condition. Non-surgical interventions, such as physical therapy, occupational therapy, and the use of assistive devices, can help improve muscle strength, flexibility, and overall function. Surgical interventions, including nerve repair and transfer procedures, may be necessary in cases where conservative treatments do not yield significant improvements or in cases of severe nerve damage. Consulting with a healthcare professional is crucial to determine the most suitable treatment option for individual cases of spinal accessory nerve damage.
Recovery and Rehabilitation from Spinal Accessory Nerve Damage
Recovering from spinal accessory nerve damage can be a gradual process that requires patience and perseverance. The extent of recovery varies from person to person based on the severity of the nerve damage and the effectiveness of the chosen treatments.
Physical Therapy and Rehabilitation
Physical therapy plays a key role in the rehabilitation process. It generally involves specialized exercises, stretches, and massage techniques to improve muscle strength, coordination, and range of motion. Rehabilitation may also include proprioceptive training, which helps individuals regain spatial awareness and proper positioning of the affected muscles.
Long-Term Prognosis and Quality of Life
While some individuals may achieve significant improvements and regain near-normal function, others may experience residual deficits. It is important to set realistic expectations and work closely with healthcare professionals to develop a tailored rehabilitation plan. Psychological support and counseling may also be beneficial in coping with any emotional or psychological effects associated with the condition.
Prevention of Spinal Accessory Nerve Damage
Prevention strategies are essential in reducing the risk of spinal accessory nerve damage.
Precautions during Surgery
If you are undergoing surgery involving the neck, head, or shoulder region, it is crucial to have an open and clear discussion with your surgeon about potential risks and complications. Understanding the surgical approach, potential nerve pathways, and postoperative care instructions can help minimize the risk of nerve damage.
Protective Measures in Daily Life
Engaging in activities that promote good posture, regular exercise, and minimizing trauma to the head, neck, and shoulder area is essential for preventing spinal accessory nerve damage. It is also advisable to consult with healthcare professionals and follow ergonomics guidelines to ensure proper body mechanics and minimize the risk of repetitive strain injuries.
In conclusion, spinal accessory nerve damage can have a profound impact on a person’s well-being and functionality. Prompt and accurate diagnosis, along with appropriate treatment and rehabilitation, can offer hope for recovery and improved quality of life. If you suspect any spinal accessory nerve-related symptoms or have concerns, it is crucial to seek medical advice and consult with a healthcare professional with experience and expertise in this field.