what foramen does the accessory nerve pass through
The accessory nerve, also known as cranial nerve XI, is an essential component of our nervous system. It plays a significant role in controlling certain muscles involved in head and neck movements. Understanding the path this nerve takes and its relationship with specific foramina (singular: foramen) is crucial for comprehending its function and potential implications of damage.
Understanding the Accessory Nerve
In order to grasp the significance of the accessory nerve’s journey through various foramina, it is vital to first familiarize ourselves with its anatomical structure and function.
Anatomy of the Accessory Nerve
The accessory nerve is composed of two primary components: the spinal accessory nerve and the cranial accessory nerve. It originates from the brainstem and spinal cord, with fibers extending from the upper spinal cord segments and cranial nerves.
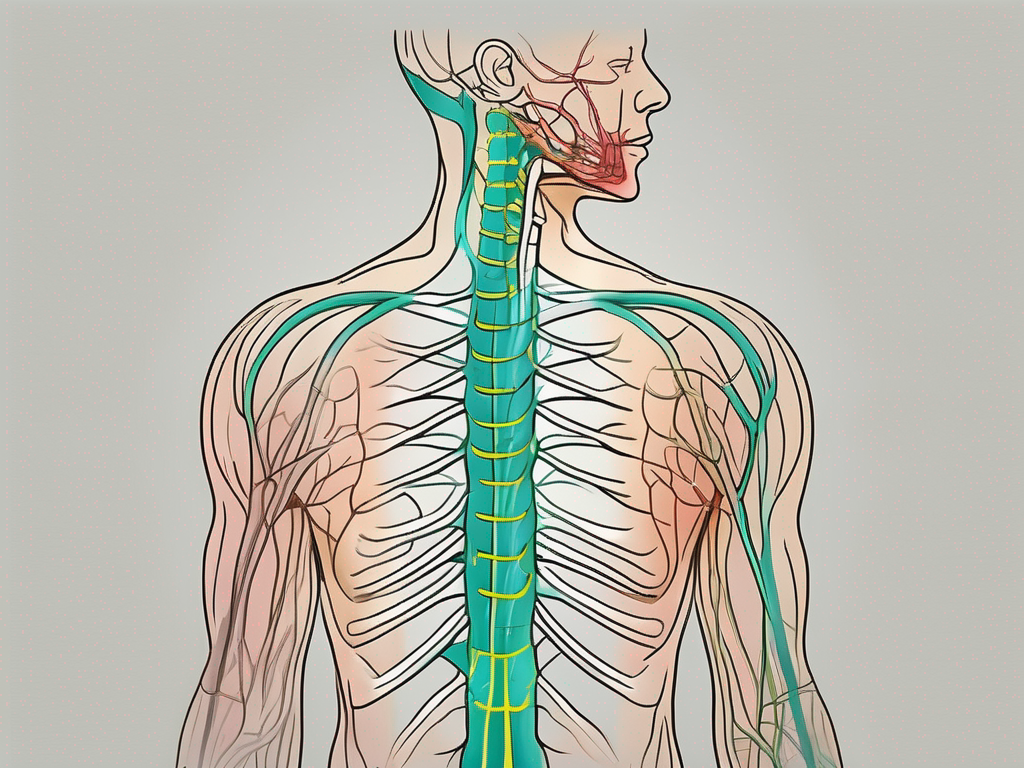
The spinal accessory nerve arises from the upper part of the spinal cord, specifically from the cervical spinal nerves (C1-C6) at the level of the spinal cord. This nerve travels through the foramen magnum, a large opening at the base of the skull, to enter the cranial cavity. From there, it descends into the posterior cranial fossa, where it joins the cranial accessory nerve.
On the other hand, the cranial accessory nerve emerges from the medulla oblongata, which is a part of the brainstem. It travels through the jugular foramen, a narrow opening located between the temporal and occipital bones of the skull. As it passes through this foramen, the cranial accessory nerve joins the spinal accessory nerve to form the accessory nerve proper.
Function of the Accessory Nerve
The accessory nerve is primarily responsible for innervating the sternocleidomastoid and trapezius muscles. These muscles are vital for various upper body movements, such as rotation and tilt of the head, as well as shoulder elevation and stabilization.
The sternocleidomastoid muscle, which is innervated by the accessory nerve, is located in the neck. It allows for the rotation of the head to the opposite side and the flexion of the neck. This muscle also plays a crucial role in maintaining proper posture and stability of the head and neck.
The trapezius muscle, also innervated by the accessory nerve, is a large muscle that extends from the base of the skull to the upper back and shoulders. It is responsible for various movements, including shoulder elevation, retraction, and rotation. The trapezius muscle also helps to stabilize the shoulder girdle and maintain proper posture.
Any damage or disruption to the accessory nerve can lead to significant functional limitations and discomfort in these muscle groups, affecting daily activities and overall quality of life. Conditions such as accessory nerve palsy, which can result from trauma, surgery, or other underlying causes, can cause weakness or paralysis of the sternocleidomastoid and trapezius muscles. Physical therapy and other rehabilitative measures are often necessary to restore function and alleviate symptoms in these cases.
The Role of Foramen in Nerve Passage
The human body is a complex system, and its various structures often interact in intricate ways. Foramina, which are openings or passageways, allow nerves, blood vessels, and other vital structures to travel through or communicate with different regions of the body.
These foramina are not just simple holes; they play a crucial role in providing connectivity within the body, allowing different systems to communicate and function harmoniously. Without these passageways, the body’s intricate network of nerves and blood vessels would not be able to function properly.
What is a Foramen?
A foramen refers to a natural opening or hole in a bone or other anatomical structures. These openings have essential functions, serving as pathways for various structures, including nerves, blood vessels, and ligaments.
Imagine the body as a bustling city, with different structures and systems representing different neighborhoods. Foramina are like the bridges and tunnels that connect these neighborhoods, allowing the smooth flow of traffic and communication between them.
Just like a city’s transportation infrastructure, foramina come in various shapes and sizes, each serving a unique purpose. Some foramina are large and prominent, while others are small and inconspicuous. Regardless of their size, they all play a vital role in maintaining the body’s overall functionality.
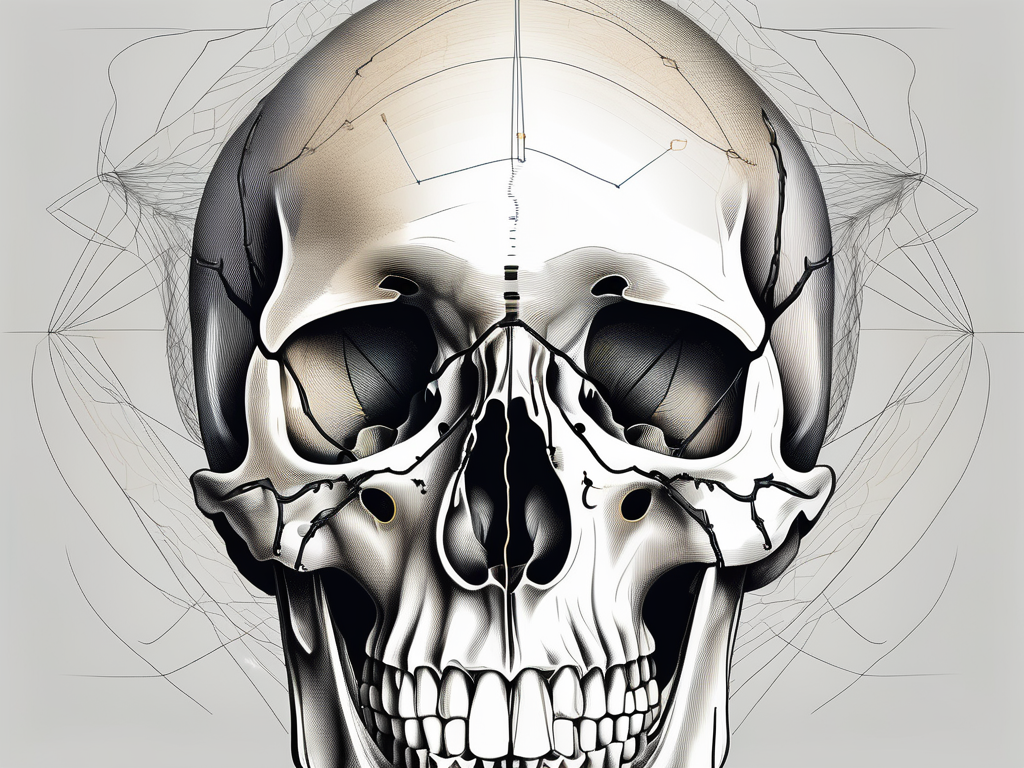
Different Types of Foramen in the Human Body
The human body contains numerous foramina, each serving a unique purpose. Some of the most prominent foramina include the foramen magnum, foramen ovale, and foramen rotundum, among others. Each specific foramen accommodates various structures, such as nerves or blood vessels.
Let’s take a closer look at the foramen magnum, which is the largest foramen in the human body. Situated at the base of the skull, it serves as a gateway between the brain and the spinal cord. This crucial passageway allows the spinal cord to connect with the brainstem, facilitating the transmission of vital information between the two.
Similarly, the foramen ovale, located in the skull’s base, plays a significant role in fetal development. During pregnancy, this foramen allows blood to bypass the lungs and flow directly from the right atrium to the left atrium of the heart. This temporary shunt ensures that the developing fetus receives oxygenated blood from the mother.
Another notable foramen is the foramen rotundum, found in the sphenoid bone. This small, circular opening serves as a pathway for the maxillary nerve, one of the major branches of the trigeminal nerve. The maxillary nerve is responsible for transmitting sensory information from the face, including pain, touch, and temperature, to the brain.
These are just a few examples of the diverse range of foramina found in the human body. Each foramen has its own unique characteristics and functions, contributing to the overall complexity and efficiency of the body’s interconnected systems.
The Accessory Nerve and the Foramen
The accessory nerve, also known as cranial nerve XI, plays a vital role in the motor control of certain muscles in the head and neck region. It originates from different regions of the central nervous system, and in order to reach its target muscles, it must navigate through specific foramina.
This interaction between the accessory nerve and foramina is critical for the overall functionality of this cranial nerve. Let’s explore in more detail the specific foramen through which the accessory nerve emerges and the journey it takes.
The Specific Foramen for the Accessory Nerve
The accessory nerve emerges through the jugular foramen, a passage located in the skull base. This foramen is positioned between the temporal bone and the occipital bone, providing access for not only the accessory nerve but also other vital structures.
In addition to the accessory nerve, the jugular foramen is shared by several other cranial nerves, including the glossopharyngeal and vagus nerves. This underscores its importance as a crucial pathway in the head and neck region, serving as a gateway for multiple essential nerves.
Through the jugular foramen, the accessory nerve exits the skull and extends downward into the neck. It traverses the sternocleidomastoid muscle, a large muscle located on the side of the neck, before innervating the trapezius muscle.
The Journey of the Accessory Nerve through the Foramen
As the accessory nerve passes through the jugular foramen, it navigates through a confined space that houses delicate structures. This intricate journey exposes the accessory nerve to potential risks and challenges.
Any abnormalities within the jugular foramen, such as compression or entrapment, can potentially cause damage or dysfunction of the accessory nerve. It is crucial for healthcare professionals to be aware of these risks and take appropriate measures to prevent or address them.
Furthermore, the accessory nerve’s passage through the foramen exposes it to various external factors that may pose a threat. Trauma, injury, or pathological processes in the surrounding area can potentially affect the functionality of the accessory nerve, leading to impairment.
Understanding the complex relationship between the accessory nerve and the foramen is essential for healthcare professionals involved in the diagnosis and treatment of conditions affecting this cranial nerve. By recognizing the potential risks and challenges associated with the accessory nerve’s journey through the foramen, they can ensure appropriate care and management to maintain optimal functionality.
Implications of Accessory Nerve Damage
Damage to the accessory nerve can have a profound impact on motion and function in the affected areas. Understanding the causes, symptoms, and appropriate treatment options is essential for managing and potentially recovering from such damage.
The accessory nerve, also known as cranial nerve XI, is responsible for controlling the movement of certain muscles in the head, neck, and shoulders. When this nerve is damaged, it can lead to significant limitations in daily activities and overall quality of life.
Causes of Accessory Nerve Damage
Accessory nerve damage can occur as a result of various factors, including trauma, surgery, tumors, or inflammation. Automobile accidents, neck injuries, and surgical procedures involving the head, neck, or shoulders pose a higher risk of accessory nerve damage.
For example, a severe whiplash injury from a car accident can cause the accessory nerve to become compressed or stretched, leading to damage. Similarly, surgical procedures that involve the removal of tumors in the neck or shoulder region can inadvertently injure the accessory nerve.
It is important to note that timely diagnosis and intervention are crucial in preventing permanent damage and promoting recovery. The sooner the damage is identified and treated, the better the chances of restoring normal function.
Symptoms and Diagnosis of Accessory Nerve Damage
The symptoms of accessory nerve damage may vary depending on the extent and location of the injury. Common signs include neck pain, weakness in the affected muscles, limited range of motion, and difficulty performing daily activities involving the head and neck.
For instance, individuals with accessory nerve damage may experience difficulty turning their head, raising their shoulders, or lifting objects above their head. They may also have trouble speaking or swallowing due to the involvement of the accessory nerve in these functions.
When experiencing such symptoms, it is vital to consult a medical professional for an accurate diagnosis. They may conduct physical examinations, imaging tests, and nerve conduction studies to evaluate the extent of the damage and determine the most appropriate treatment approach.
During a physical examination, the healthcare provider may assess muscle strength, range of motion, and reflexes in the affected areas. They may also order imaging tests, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, to visualize the structures and identify any abnormalities or injuries.
In addition, nerve conduction studies may be performed to assess the electrical activity of the accessory nerve and determine if there is any disruption in the nerve signals. This test involves placing electrodes on the skin and measuring the speed and strength of the nerve impulses.
Overall, an accurate diagnosis is crucial for developing an effective treatment plan tailored to the individual’s specific needs and goals. Treatment options may include physical therapy, medication, nerve stimulation techniques, or, in severe cases, surgical intervention.
Physical therapy plays a vital role in accessory nerve damage rehabilitation. A skilled physical therapist can design a customized exercise program to improve muscle strength, range of motion, and overall functional abilities. They may also incorporate techniques such as manual therapy, stretching, and electrical stimulation to enhance recovery.
Medication, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants, may be prescribed to manage pain and reduce inflammation in the affected areas. Additionally, nerve stimulation techniques, such as transcutaneous electrical nerve stimulation (TENS) or neuromuscular electrical stimulation (NMES), can help promote nerve regeneration and improve muscle function.
In severe cases where conservative measures fail to provide relief, surgical intervention may be considered. The specific surgical procedure will depend on the underlying cause and extent of the damage. The goal of surgery is to repair or reconstruct the damaged accessory nerve, allowing for improved function and symptom relief.
Recovery from accessory nerve damage can vary depending on the individual and the severity of the injury. It may take weeks to months of consistent treatment and rehabilitation to regain optimal function. However, with proper medical care and rehabilitation, many individuals can experience significant improvement and resume their normal activities.
In conclusion, accessory nerve damage can have a significant impact on motion and function in the affected areas. Timely diagnosis, appropriate treatment, and rehabilitation are essential for managing and potentially recovering from such damage. By understanding the causes, symptoms, and treatment options, individuals with accessory nerve damage can take proactive steps towards regaining their quality of life.
Treatment and Recovery for Accessory Nerve Damage
The accessory nerve, also known as cranial nerve XI, is a crucial component of our nervous system, supporting essential head and neck movements. It originates from the brainstem and passes through the jugular foramen, a small opening in the base of the skull. This nerve plays a vital role in controlling the movement of certain muscles, such as those responsible for shrugging the shoulders and turning the head.
Medical Interventions for Accessory Nerve Damage
When it comes to treating accessory nerve damage, the approach depends on various factors, including the underlying cause, the severity of the injury, and individual circumstances. It is crucial to consult with a healthcare provider to determine the best course of action.
In many cases, conservative management techniques are employed to help restore strength, flexibility, and functionality. Physical therapy, for example, can be an effective treatment option. Skilled therapists can guide individuals through targeted exercises and techniques focused on neck and shoulder mobility, muscle strengthening, and pain management. These interventions aim to promote healing and improve overall function.
For more severe cases of accessory nerve damage, surgical interventions may be necessary. Surgeons can repair or reconstruct the damaged nerve, helping to restore its normal function. However, it is important to note that the timeline and extent of recovery can vary for each individual case.
Patience, compliance with recommended treatments, and close collaboration with healthcare professionals are key factors in maximizing recovery outcomes. It is essential to follow the prescribed treatment plan and attend regular follow-up appointments to monitor progress and make any necessary adjustments.
Rehabilitation and Recovery Process
Rehabilitation programs tailored to the individual’s specific needs and goals play a vital role in the recovery process. Physical therapy, in particular, can be instrumental in restoring function and alleviating discomfort.
Working closely with skilled therapists, individuals can learn techniques to compensate for any persistent limitations and gradually regain independence and quality of life. These programs often include a combination of exercises, manual therapy, and modalities such as heat or cold therapy, electrical stimulation, and ultrasound.
While every effort is made to promote healing, it is important to recognize that complete restoration of pre-injury function may not always be possible. In such cases, adaptive strategies and assistive devices can aid individuals in adapting to any permanent changes and continuing to lead fulfilling lives.
Psychological support is also an essential component of the rehabilitation process. Coping with the physical and emotional challenges that accompany nerve damage can be overwhelming. Mental health professionals can provide guidance and support to help individuals navigate these difficulties and maintain a positive mindset throughout their recovery journey.
In conclusion, the accessory nerve is a vital component of our nervous system, supporting essential head and neck movements. Its passage through the jugular foramen underscores the importance of understanding the relationship between cranial nerves and specific foramina. Accessory nerve damage can significantly impact daily functioning, but timely diagnosis, appropriate treatment, and dedicated rehabilitation can help individuals regain their independence and enhance their overall well-being.
If you suspect any accessory nerve-related issues, such as weakness or limited range of motion in the neck and shoulders, consult with a healthcare professional for an accurate diagnosis and tailored treatment plan. Remember, early intervention is key to achieving the best possible outcome.