what causes dysfunction of accessory nerve
The accessory nerve, also known as cranial nerve XI, plays a crucial role in the functioning of our neck and shoulder muscles. Dysfunction of this nerve can lead to pain, weakness, and limited movement in these areas, greatly impacting our daily lives. In this article, we will explore the various causes of accessory nerve dysfunction, symptoms to watch out for, diagnostic procedures, available treatment options, and tips to prevent and manage this condition effectively.
Understanding the Accessory Nerve
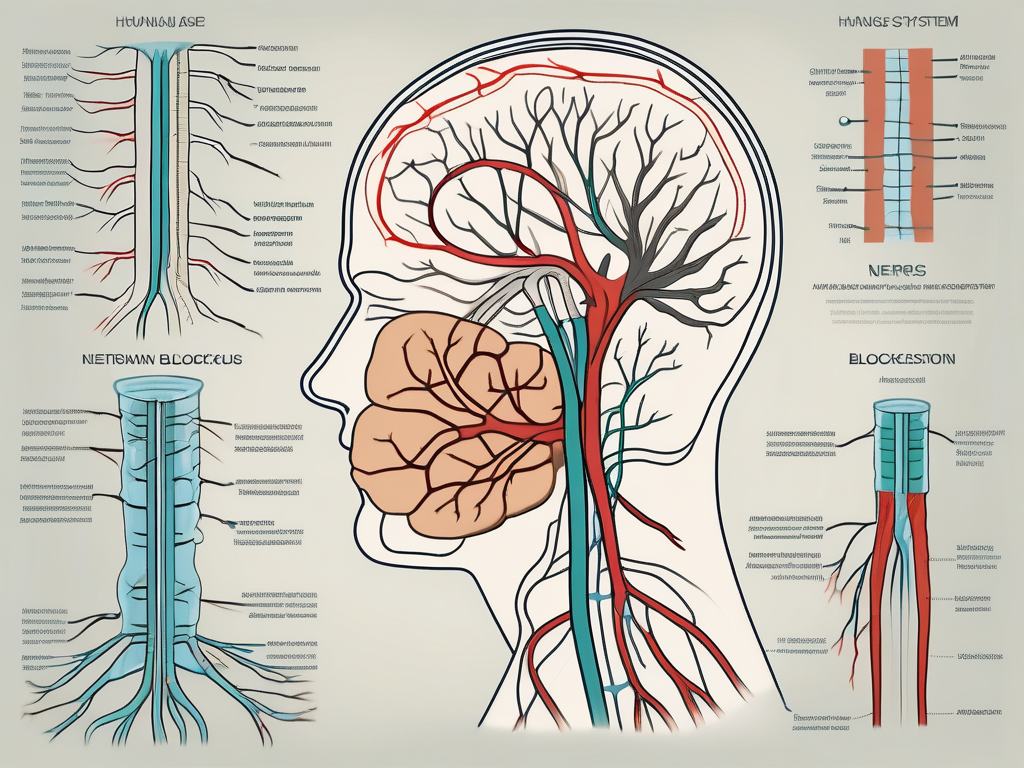
The accessory nerve, also known as the eleventh cranial nerve, plays a crucial role in coordinating the movement of our neck and shoulder muscles. It is a paired cranial nerve that originates in the upper spinal cord and extends to the neck and shoulder muscles. The accessory nerve consists of two components: the spinal accessory nerve and the cranial accessory nerve.
Anatomy of the Accessory Nerve
The spinal accessory nerve, one of the components of the accessory nerve, arises from the upper spinal cord, specifically from the motor neurons in the ventral horn of the cervical spinal cord segments. It then ascends through the foramen magnum, the large opening at the base of the skull, and enters the cranial cavity.
Within the cranial cavity, the spinal accessory nerve joins forces with the cranial accessory nerve, which originates from the nucleus ambiguus in the medulla oblongata, a part of the brainstem. The two components of the accessory nerve then exit the skull through the jugular foramen, a small opening located between the temporal bone and the occipital bone.
Once outside the skull, the accessory nerve descends into the neck, where it innervates specific neck muscles. It provides motor control to muscles such as the sternocleidomastoid, which allows us to turn our head, and the trapezius, which enables us to shrug our shoulders.
Function of the Accessory Nerve
The primary function of the accessory nerve is to coordinate the movement of our neck and shoulder muscles. It works in conjunction with other cranial nerves, such as the facial nerve and the glossopharyngeal nerve, to ensure smooth and coordinated movements.
When the accessory nerve is functioning optimally, these movements are effortless, allowing us to perform daily activities without pain or discomfort. For example, when we turn our head to look at something, the accessory nerve works in tandem with other muscles and nerves to execute the movement smoothly and precisely.
In addition to facilitating head movements, the accessory nerve also plays a vital role in shoulder movement. It innervates the trapezius muscle, which is responsible for elevating, retracting, and rotating the scapula. This allows us to perform actions such as shrugging our shoulders, lifting objects, and reaching overhead.
It is worth noting that damage or dysfunction of the accessory nerve can result in various symptoms, including weakness or paralysis of the affected muscles. This can lead to difficulties in performing everyday tasks that require neck and shoulder movements.
In conclusion, the accessory nerve is a crucial component of our nervous system, enabling us to move our neck and shoulder muscles with precision and ease. Its intricate anatomy and coordinated function contribute to our ability to perform a wide range of activities in our daily lives.
Common Symptoms of Accessory Nerve Dysfunction
Physical Symptoms
Individuals with accessory nerve dysfunction may experience a range of physical symptoms. These can include neck and shoulder pain, muscle weakness, stiffness, and difficulty moving the head or shoulders. In severe cases, muscle wasting may occur due to prolonged inactivity.
Neck and shoulder pain can vary in intensity and location. Some individuals may experience a dull, aching pain that radiates from the neck to the shoulders, while others may have sharp, shooting pains that limit their range of motion. The pain can be constant or intermittent, and it may worsen with certain movements or activities.
Muscle weakness is another common symptom of accessory nerve dysfunction. This weakness can affect the muscles in the neck, shoulders, and upper back, making it difficult to perform everyday tasks that require strength, such as lifting heavy objects or carrying groceries. The weakness may also lead to fatigue and a general feeling of physical exhaustion.
Stiffness in the neck and shoulders is often experienced by individuals with accessory nerve dysfunction. This stiffness can make it challenging to turn the head from side to side or tilt it up and down. It may feel as though the muscles are tight and resistant to movement, causing discomfort and limited mobility.
Difficulty moving the head or shoulders is a significant symptom of accessory nerve dysfunction. Individuals may find it hard to rotate their head fully or lift their shoulders properly. This limitation in movement can affect daily activities such as driving, looking over one’s shoulder, or participating in sports that require upper body mobility.
In severe cases of accessory nerve dysfunction, muscle wasting may occur due to prolonged inactivity. When the muscles are not used regularly, they can begin to weaken and shrink. This can further exacerbate the symptoms of pain, weakness, and limited mobility.
Impact on Daily Activities
Accessory nerve dysfunction can significantly impact daily activities. Simple tasks such as driving, lifting objects, and even turning the head to engage in conversations can become challenging and painful. The limitations in movement and strength can affect one’s ability to perform essential activities of daily living.
Driving can be particularly difficult for individuals with accessory nerve dysfunction. The need to turn the head to check blind spots or look over the shoulder can be painful and limited. This can make driving unsafe and increase the risk of accidents. It is crucial for individuals experiencing these symptoms to seek medical attention and explore alternative transportation options if necessary.
Lifting objects, whether they are heavy or not, can also be a challenge for those with accessory nerve dysfunction. The weakness and limited mobility in the neck, shoulders, and upper back can make it difficult to lift objects properly and without pain. This can impact one’s ability to perform household chores, carry groceries, or engage in physical activities.
Engaging in conversations can become uncomfortable for individuals with accessory nerve dysfunction. The limited ability to turn the head or lift the shoulders can make it challenging to maintain eye contact or participate in group discussions. This can lead to feelings of social isolation and frustration.
Overall, the impact of accessory nerve dysfunction on daily activities can be significant. It is essential to seek medical attention if these symptoms persist or worsen over time. Early intervention and appropriate treatment can help manage the symptoms and improve quality of life.
Causes of Accessory Nerve Dysfunction
The accessory nerve, also known as cranial nerve XI, plays a crucial role in motor function, specifically in controlling the movement of certain muscles in the head, neck, and shoulder area. Dysfunction of this nerve can have various causes, ranging from trauma-related incidents to medical conditions.
Trauma-Related Causes
Physical trauma is one of the leading causes of accessory nerve dysfunction. Injuries to the head, neck, or shoulder area can result in damage to the nerve, leading to impaired functionality. Motor vehicle accidents, sports injuries, falls, and blunt force trauma are common culprits.
When a traumatic incident occurs, the accessory nerve may be stretched, compressed, or even severed. The force exerted on the nerve can disrupt its normal function, causing weakness or paralysis in the affected muscles. Rehabilitation and physical therapy are often necessary to regain muscle strength and restore movement.
Medical Conditions Leading to Dysfunction
While trauma-related causes are prevalent, various medical conditions can also contribute to accessory nerve dysfunction. One such condition is the presence of tumors in the neck or surrounding areas. These tumors can exert pressure on the nerve, compromising its function. Neck tumors, in particular, can pose a significant risk to the accessory nerve due to their proximity.
Infections can also play a role in accessory nerve dysfunction. Lyme disease, a tick-borne illness, is known to affect nerve health and can lead to impairments in the accessory nerve. Additionally, viral infections can cause inflammation and damage to the nerve, resulting in dysfunction.
Furthermore, nerve entrapment or impingement syndromes can contribute to accessory nerve dysfunction. These conditions occur when a nerve becomes compressed or trapped, leading to pain, weakness, and limited mobility. In the case of the accessory nerve, entrapment or impingement can disrupt its normal function, affecting the muscles it controls.
It is important to note that accessory nerve dysfunction can manifest in various ways, depending on the severity of the injury or underlying condition. Symptoms may include difficulty moving the head, neck, or shoulder, muscle weakness, pain, and limited range of motion. Proper diagnosis and treatment by a medical professional are essential for managing and addressing accessory nerve dysfunction.
Diagnosis of Accessory Nerve Dysfunction
The diagnosis of accessory nerve dysfunction involves a series of clinical examination procedures and, in some cases, imaging and laboratory tests. A healthcare provider will carefully evaluate the range of motion, strength, and reflexes of the affected muscles during the clinical examination. This assessment helps in determining whether accessory nerve dysfunction is the underlying cause of the symptoms.
During the clinical examination, the healthcare provider will also inquire about the patient’s symptoms, medical history, and any recent injuries. This comprehensive evaluation allows for a better understanding of the patient’s condition and helps in making an accurate diagnosis.
Clinical Examination Procedures
The clinical examination for accessory nerve dysfunction involves various procedures to assess the affected muscles. The healthcare provider will carefully observe the patient’s movements, looking for any limitations or abnormalities in the range of motion. They may ask the patient to perform specific movements, such as shrugging the shoulders or turning the head, to evaluate the strength and coordination of the muscles controlled by the accessory nerve.
In addition to evaluating the range of motion and strength, the healthcare provider will also test the reflexes of the affected muscles. By tapping on specific areas, such as the trapezius muscle, the healthcare provider can assess the reflex response and determine if there is any dysfunction of the accessory nerve.
Imaging and Laboratory Tests
In some cases, imaging tests may be ordered to further evaluate accessory nerve dysfunction. An MRI (magnetic resonance imaging) or CT (computed tomography) scan can provide detailed images of the neck, shoulder, and surrounding areas. These imaging tests can help identify any structural abnormalities or nerve damage that may be contributing to the dysfunction.
Additionally, blood tests may be conducted to rule out any underlying autoimmune diseases or infections that could be causing or contributing to the accessory nerve dysfunction. These tests can help identify any markers of inflammation or infection in the body, providing valuable information for the diagnosis and treatment of the condition.
It is important to note that the specific diagnostic procedures may vary depending on the individual case and the healthcare provider’s clinical judgment. The goal of the diagnostic process is to accurately identify the cause of the symptoms and develop an appropriate treatment plan tailored to the patient’s needs.
Treatment Options for Accessory Nerve Dysfunction
Accessory nerve dysfunction, also known as spinal accessory nerve palsy, can cause significant discomfort and limitations in daily activities. Fortunately, there are various treatment options available to manage this condition and improve overall quality of life.
Non-Surgical Treatments
The initial treatment approach for accessory nerve dysfunction typically involves non-surgical interventions. These treatments aim to alleviate symptoms, improve muscle strength and range of motion, and enhance overall functionality.
Physical therapy is often recommended as a first-line treatment for accessory nerve dysfunction. A skilled physical therapist will design a personalized exercise program to target the affected muscles and promote their recovery. These exercises may include stretching, strengthening, and range of motion exercises to improve muscle function and reduce pain.
In addition to physical therapy, pain management techniques can also be employed to provide relief. Heat therapy, such as the application of warm compresses or hot packs, can help relax tense muscles and alleviate discomfort. Nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain medications may also be prescribed to manage pain and inflammation.
Furthermore, lifestyle modifications can play a crucial role in the management of accessory nerve dysfunction. Avoiding activities that strain the affected muscles, such as heavy lifting or repetitive motions, can help prevent further damage and promote healing. Ergonomic adjustments, such as using proper posture and supportive devices, may also be recommended to reduce strain on the affected muscles.
It is important to note that the treatment plan for accessory nerve dysfunction should be tailored to individual needs. Consulting with a healthcare professional, such as a neurologist or physical therapist, is essential to receive proper guidance and ensure the most effective treatment approach.
Surgical Interventions
In severe cases or when conservative treatments do not yield significant improvement, surgical intervention may be considered. Surgery aims to alleviate pressure on the nerve, repair any damage, and restore normal functionality.
The specific surgical approach for accessory nerve dysfunction will depend on the underlying cause and extent of nerve damage. In some cases, decompression surgery may be performed to relieve pressure on the nerve caused by surrounding structures. This can involve removing or repositioning structures that are compressing the nerve, such as scar tissue or tumors.
In situations where the accessory nerve has been severely damaged or severed, nerve repair or grafting procedures may be necessary. These surgical techniques involve reconnecting or replacing damaged nerve segments to restore function and promote nerve regeneration.
It is important to consult with a specialist, such as a neurosurgeon or orthopedic surgeon, to determine the best course of action for surgical intervention. They will assess the individual’s specific condition and recommend the most appropriate surgical approach.
In conclusion, accessory nerve dysfunction can be effectively managed through a combination of non-surgical and surgical treatments. Non-surgical interventions, such as physical therapy, pain management techniques, and lifestyle modifications, are often the first line of treatment. However, in severe cases, surgical intervention may be necessary to alleviate pressure on the nerve and restore normal functionality. Consulting with healthcare professionals is crucial to receive proper guidance and ensure the most effective treatment approach for accessory nerve dysfunction.
Prevention and Management of Accessory Nerve Dysfunction
Lifestyle Modifications
To reduce the risk of accessory nerve dysfunction, it is important to adopt healthy habits and practices. This can include maintaining proper posture, avoiding repetitive or strenuous activities that strain the neck and shoulder muscles, and implementing regular exercise routines that focus on strengthening these areas. It is also essential to take breaks when engaged in activities that require prolonged neck or shoulder involvement.
Proper posture plays a significant role in preventing accessory nerve dysfunction. When sitting or standing, it is crucial to keep the spine aligned and the shoulders relaxed. Slouching or hunching over can put unnecessary strain on the neck and shoulder muscles, increasing the risk of nerve dysfunction. By consciously maintaining good posture throughout the day, individuals can alleviate stress on the accessory nerve and reduce the likelihood of developing related issues.
Avoiding repetitive or strenuous activities that strain the neck and shoulder muscles is another key aspect of prevention. Jobs or hobbies that involve constant overhead reaching, heavy lifting, or repetitive motions can put excessive pressure on the accessory nerve, leading to dysfunction over time. It is important to be mindful of these activities and take necessary precautions, such as using proper lifting techniques, taking frequent breaks, and alternating tasks to distribute the workload evenly.
Incorporating regular exercise routines that focus on strengthening the neck and shoulder muscles can significantly contribute to preventing accessory nerve dysfunction. Exercises that target these areas, such as shoulder shrugs, neck stretches, and resistance training, can help build strength and improve muscle endurance. Stronger muscles provide better support to the accessory nerve, reducing the risk of compression or injury.
Taking breaks when engaged in activities that require prolonged neck or shoulder involvement is crucial for preventing accessory nerve dysfunction. Whether it’s working on a computer, painting, or playing a musical instrument, it is important to give the muscles a chance to rest and recover. Taking short breaks every 30 minutes or so can help alleviate muscle tension and prevent overuse injuries that can affect the accessory nerve.
Physical Therapy and Rehabilitation
Engaging in physical therapy and rehabilitation programs can greatly aid in the prevention and management of accessory nerve dysfunction. These programs focus on strengthening the affected muscles, improving range of motion, and providing pain relief. A qualified physical therapist can develop an individualized treatment plan to address specific needs and goals.
Physical therapy sessions for accessory nerve dysfunction often include a combination of exercises, manual therapy techniques, and modalities such as heat or cold therapy. The exercises are designed to target the affected muscles and improve their strength and flexibility. Manual therapy techniques, such as massage and joint mobilization, can help reduce muscle tension and improve blood circulation in the affected area. Modalities like heat or cold therapy can provide pain relief and reduce inflammation.
In addition to in-clinic sessions, physical therapists may also provide patients with home exercise programs to continue their rehabilitation outside of the clinic. These programs typically include a range of exercises that can be performed at home with minimal equipment. Adhering to these programs can help individuals maintain the progress made during therapy sessions and further strengthen the accessory nerve and surrounding muscles.
Physical therapy and rehabilitation can also play a crucial role in managing accessory nerve dysfunction after it has already occurred. Through targeted exercises and therapies, individuals can regain strength, improve range of motion, and reduce pain associated with the dysfunction. Regular follow-up appointments with the physical therapist can ensure that progress is being made and any necessary adjustments to the treatment plan can be made.
In conclusion, dysfunction of the accessory nerve can be caused by various factors, including trauma, medical conditions, and infections. Recognizing the symptoms, seeking proper diagnosis, and exploring available treatment options are essential steps towards managing this condition effectively. However, it is crucial to consult with a healthcare professional for personalized advice and guidance. By understanding the causes and taking preventive measures, individuals can maintain optimal nerve health and enjoy a pain-free range of motion in their neck and shoulder muscles.


