what can damage the accessory nerve
The accessory nerve, also known as the 11th cranial nerve, plays a crucial role in the movement of the head, neck, and shoulders. Damage to this nerve can lead to significant impairments in daily activities and overall quality of life. In this article, we will explore the various factors that can cause damage to the accessory nerve, along with the symptoms, diagnostic procedures, treatment options, prevention strategies, and the long-term outlook for individuals with accessory nerve damage.
Understanding the Accessory Nerve
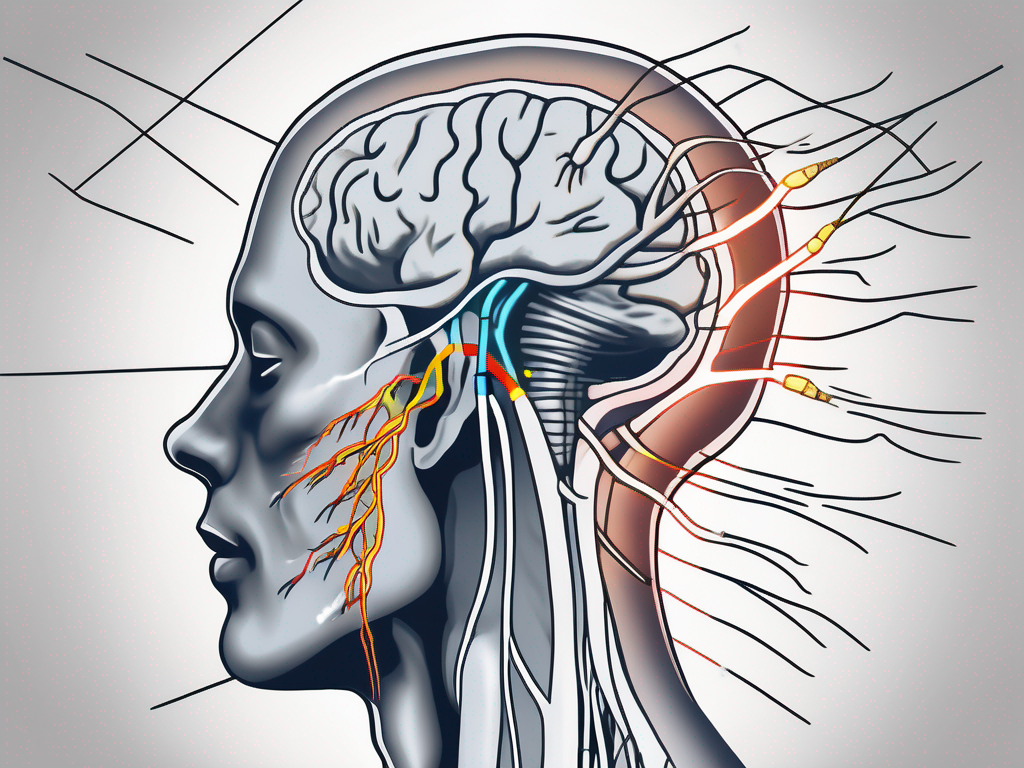
The accessory nerve is a motor nerve that arises from the brainstem and travels down to the muscles of the neck and shoulder. It consists of two parts – the cranial part, originating from the medulla oblongata, and the spinal part, arising from the upper cervical spinal cord segments. This nerve innervates important muscles, including the sternocleidomastoid and trapezius muscles, which are vital for movements involving head rotation, shrugging, and various shoulder movements.
Anatomy of the Accessory Nerve
The accessory nerve has a complex anatomy, with the cranial part being primarily responsible for innervating the muscles involved in head rotation, while the spinal part predominantly controls the muscles responsible for shoulder movements.
The cranial part of the accessory nerve originates from the medulla oblongata, which is located at the base of the brainstem. It travels through the jugular foramen, a small opening in the skull, and then branches out to innervate the sternocleidomastoid muscle. This muscle, located on the sides of the neck, plays a crucial role in head rotation and flexion.
The spinal part of the accessory nerve arises from the upper cervical spinal cord segments, specifically from the ventral rootlets of the first five cervical nerves. It joins the cranial part of the accessory nerve and descends through the neck, passing through the posterior triangle of the neck. It then innervates the trapezius muscle, a large muscle that extends from the base of the skull to the upper back and shoulders. The trapezius muscle is responsible for movements such as shrugging, retracting the scapulae, and stabilizing the shoulders.
Function of the Accessory Nerve
The primary function of the accessory nerve is to coordinate movements of the head, neck, and shoulders. It works in conjunction with other nerves, such as the facial nerve, to ensure smooth and coordinated muscle actions necessary for everyday activities.
When the accessory nerve is functioning properly, it allows for effortless head rotation, enabling us to look in different directions. It also facilitates movements like nodding, tilting, and flexing the head. Additionally, the accessory nerve plays a crucial role in shoulder movements, allowing us to raise our shoulders, retract the scapulae, and perform various arm movements.
Damage or dysfunction of the accessory nerve can lead to significant impairments in head and shoulder movements. For example, if the cranial part of the accessory nerve is affected, it can result in difficulty turning the head or tilting it to the side. On the other hand, damage to the spinal part of the accessory nerve can lead to weakness or paralysis of the trapezius muscle, causing shoulder drooping and limited range of motion.
Injuries to the accessory nerve can occur due to trauma, surgical procedures, or certain medical conditions. Physical therapy and rehabilitation techniques are often employed to help individuals regain optimal function and mobility of the head, neck, and shoulders.
Common Causes of Accessory Nerve Damage
Several factors can lead to damage to the accessory nerve. Understanding these causes can help individuals identify potential risk factors and take appropriate measures to prevent such damage.
The accessory nerve, also known as the eleventh cranial nerve, plays a crucial role in controlling certain muscles in the neck and shoulder region. Damage to this nerve can result in functional impairments and difficulties in performing daily activities.
Trauma and Injuries
Traumatic events, such as motor vehicle accidents, falls, or sports injuries, can result in direct damage to the accessory nerve. The force exerted on the neck and shoulder region during these events can cause nerve compression, stretching, or even complete severance, leading to functional impairments.
For example, in a motor vehicle accident, the sudden impact can cause the head and neck to jerk forcefully, potentially damaging the accessory nerve. Similarly, a fall from a height can result in a direct blow to the shoulder or neck, leading to nerve injury.
It is important to note that the severity of the trauma does not always correlate with the extent of nerve damage. Even seemingly minor incidents can cause significant harm to the accessory nerve, highlighting the need for caution and preventive measures in various activities.
Surgical Complications
In some cases, surgical procedures involving the neck or shoulder region can inadvertently damage the accessory nerve. This can occur during procedures such as neck dissections, lymph node removal, or surgeries to correct shoulder instability. Careful attention and skillful execution are crucial during these procedures to minimize the risk of nerve damage.
During a neck dissection, for instance, the surgeon must navigate through delicate structures to remove lymph nodes or tumors. In doing so, there is a potential risk of inadvertently damaging the accessory nerve, which runs in close proximity to these structures.
Surgeries to correct shoulder instability, such as a Bankart repair, also carry a risk of accessory nerve damage. The surgeon must manipulate the shoulder joint and surrounding tissues, increasing the chances of nerve injury if not performed with precision.
Neurological Disorders
Certain neurological conditions, such as amyotrophic lateral sclerosis (ALS) or cervical spinal cord tumors, can also contribute to the damage of the accessory nerve. These conditions may affect the nerve directly or lead to compression or infiltration, resulting in functional impairments.
In ALS, a progressive neurodegenerative disease, the motor neurons responsible for controlling muscle movement gradually degenerate. This can affect the accessory nerve, leading to weakness or paralysis of the muscles it innervates.
Cervical spinal cord tumors, on the other hand, can exert pressure on the accessory nerve as they grow, causing nerve dysfunction. The tumor may compress the nerve directly or disrupt its normal function by infiltrating the surrounding tissues.
It is important for individuals with neurological disorders to receive appropriate medical care and management to minimize the impact on the accessory nerve and maintain optimal function.
Symptoms of Accessory Nerve Damage
The symptoms of accessory nerve damage can vary depending on the extent and location of the injury. It is important to note that these symptoms may not be exclusive to accessory nerve damage and can be associated with other medical conditions as well. Consulting with a healthcare professional is crucial for an accurate diagnosis.
Physical Symptoms
Individuals with accessory nerve damage may experience weakness or paralysis in the affected muscles. This can manifest as difficulty in turning the head, lifting the shoulders, or performing everyday tasks that involve these muscles. Pain and muscle stiffness may also be present in some cases.
When the accessory nerve, also known as cranial nerve XI, is damaged, it can affect the function of the sternocleidomastoid and trapezius muscles. These muscles are responsible for various movements of the head, neck, and shoulders. When the accessory nerve is compromised, it can result in limited range of motion and weakness in these areas.
For example, individuals with accessory nerve damage may find it challenging to turn their head from side to side. This can make simple tasks like checking blind spots while driving or looking over the shoulder while crossing the street more difficult and potentially dangerous.
In addition to head movements, accessory nerve damage can also affect the ability to lift the shoulders. This can impact daily activities such as carrying heavy objects, reaching for items on high shelves, or participating in sports that require upper body strength.
Furthermore, individuals with accessory nerve damage may experience pain and muscle stiffness. This can occur due to the muscles being unable to function properly, leading to strain and tension. The pain may be localized to the affected muscles or radiate to surrounding areas.
Cognitive and Emotional Effects
In addition to physical symptoms, accessory nerve damage can have cognitive and emotional effects on individuals. The impact of limited mobility and functional impairment can lead to frustration, decreased self-esteem, and feelings of isolation. These psychological effects can significantly affect an individual’s overall well-being.
When individuals are unable to perform daily tasks that were once effortless, it can be emotionally distressing. Simple activities like grooming, dressing, or even holding a conversation can become challenging and frustrating. This can lead to a decrease in self-esteem as individuals may feel dependent on others for assistance.
Feelings of isolation can also arise as individuals may avoid social situations due to the limitations imposed by accessory nerve damage. They may fear judgment or embarrassment, leading to a withdrawal from social activities and a sense of loneliness.
Furthermore, the cognitive effects of accessory nerve damage can include difficulties with concentration and memory. The emotional toll of dealing with chronic pain, physical limitations, and the impact on daily life can make it challenging to focus and remember information.
It is important for individuals with accessory nerve damage to seek support from healthcare professionals, as they can provide guidance and strategies to manage the cognitive and emotional effects of the condition. Physical therapy and rehabilitation programs can also play a crucial role in improving mobility and overall well-being.
Diagnostic Procedures for Accessory Nerve Damage
Accurate diagnosis of accessory nerve damage is crucial to determine the appropriate treatment and management strategies. Healthcare professionals may use several diagnostic procedures to assess the extent and location of nerve damage.
When a patient presents with symptoms that suggest accessory nerve damage, healthcare professionals employ a variety of diagnostic techniques to gather information and make an accurate diagnosis. These procedures not only help identify the presence of accessory nerve damage but also provide valuable insights into the underlying causes and potential treatment options.
Medical History and Physical Examination
During the initial assessment, the healthcare professional will gather detailed information about the individual’s medical history and perform a comprehensive physical examination. This helps in identifying any underlying medical conditions or previous injuries that could contribute to the accessory nerve damage.
The medical history may reveal important information about the patient’s lifestyle, occupation, and any recent trauma or infections that could have affected the accessory nerve. Additionally, the physical examination allows the healthcare professional to assess the patient’s range of motion, muscle strength, and any visible signs of nerve damage, such as muscle atrophy or abnormal muscle contractions.
Imaging Techniques
Various imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may be utilized to visualize the nerve and surrounding structures. These diagnostic tools aid in identifying any structural abnormalities or signs of nerve compression.
An MRI scan provides detailed images of the soft tissues, allowing healthcare professionals to assess the condition of the accessory nerve and identify any potential causes of damage, such as tumors or herniated discs. Similarly, a CT scan provides a cross-sectional view of the affected area, helping to identify any bony abnormalities or structural changes that may be affecting the nerve.
Neurological Tests
Neurological tests, including electromyography (EMG) and nerve conduction studies (NCS), provide valuable insights into the electrical activity and functioning of nerves and muscles. These tests can assist in assessing the integrity and functionality of the accessory nerve and help differentiate it from other nerve-related conditions.
During an EMG, small electrodes are inserted into the muscles to measure their electrical activity. This test helps determine if the accessory nerve is functioning properly and if there are any abnormalities in the muscle response. NCS, on the other hand, involves the application of small electrical shocks to the nerve to measure its conduction speed and assess its overall health.
In addition to these tests, healthcare professionals may also perform a nerve biopsy, where a small sample of the affected nerve is removed and examined under a microscope. This procedure can provide further insights into the nature and extent of the nerve damage.
Overall, the diagnostic procedures for accessory nerve damage involve a comprehensive approach that combines medical history, physical examination, imaging techniques, and neurological tests. By employing these techniques, healthcare professionals can accurately diagnose accessory nerve damage and develop an appropriate treatment plan tailored to the individual’s needs.
Treatment Options for Accessory Nerve Damage
Treatment options for accessory nerve damage focus on alleviating symptoms, improving functional abilities, and promoting overall well-being. The healthcare professional will develop an individualized treatment plan based on the specific needs and goals of the patient.
Medication and Drug Therapy
In some cases, medication may be prescribed to manage pain, reduce inflammation, or improve muscle strength and function. However, it is important to note that medications alone cannot repair or restore nerve damage, and their effectiveness may vary from person to person.
Physical and Occupational Therapy
Physical and occupational therapy play a crucial role in the rehabilitation process for individuals with accessory nerve damage. These therapies focus on strengthening the affected muscles, improving range of motion, enhancing coordination, and adapting daily activities to optimize functional abilities.
Surgical Interventions
In severe cases of accessory nerve damage, surgical interventions may be considered. These procedures aim to repair or reconstruct the damaged nerve or restore function through alternate means, such as tendon transfers. Surgical interventions are typically reserved for individuals with significant impairments or failed conservative treatments.
Prevention Strategies for Accessory Nerve Damage
While it may not always be possible to prevent accessory nerve damage, certain measures can help reduce the risk of injury or maximize recovery in case of nerve damage.
Safety Measures and Precautions
Practicing safety measures, such as wearing appropriate protective gear during sports or using proper lifting techniques, can minimize the risk of traumatic injuries to the neck and shoulder region. Additionally, maintaining a safe environment and taking precautions to avoid falls can help prevent accidents that could potentially damage the accessory nerve.
Regular Health Check-ups
Regular health check-ups and screenings can aid in early detection and management of underlying medical conditions that may contribute to accessory nerve damage. Timely intervention and appropriate management strategies are crucial in minimizing the risk of complications and optimizing outcomes.
Healthy Lifestyle Choices
Adopting a healthy lifestyle, including regular physical exercise, a balanced diet, and adequate rest, can promote overall physical and mental well-being. Engaging in activities that strengthen the muscles of the neck and shoulders can help maintain their strength and flexibility, reducing the risk of injuries.
The Long-Term Outlook for Accessory Nerve Damage
The long-term outlook for individuals with accessory nerve damage can vary depending on various factors, including the extent of the injury, promptness of diagnosis and treatment, and individual response to therapies. While some individuals may experience significant recovery and restoration of function, others may have to adapt to long-term impairments.
Recovery and Rehabilitation
Recovery and rehabilitation following accessory nerve damage can be a gradual process. Physical and occupational therapy play a vital role in promoting muscle strength, coordination, and functional abilities. It is important to set realistic expectations and work closely with healthcare professionals to maximize the recovery potential.
Potential Complications and Challenges
Individuals with accessory nerve damage may face certain complications and challenges throughout their journey. This may include persistent pain, reduced range of motion, muscle imbalances, and emotional difficulties. Regular follow-up with healthcare professionals and adherence to prescribed treatment plans can help address these challenges effectively.
Living with Accessory Nerve Damage
Living with accessory nerve damage may require adapting to certain limitations and making necessary lifestyle adjustments. Seeking support from healthcare professionals, support groups, and loved ones can provide valuable guidance and emotional support during this process, helping individuals lead fulfilling lives despite the challenges.
In conclusion, accessory nerve damage can have a significant impact on an individual’s physical and emotional well-being. Understanding the various causes, symptoms, diagnostic procedures, treatment options, and prevention strategies associated with accessory nerve damage can empower individuals to take proactive measures and seek appropriate medical care. It is crucial to consult with a healthcare professional for an accurate diagnosis and personalized treatment plan tailored to individual needs. With proper management and support, individuals with accessory nerve damage can navigate their journey towards improved function and overall well-being.


