what are the clinical presentations of the accessory nerve?
The clinical presentations of the accessory nerve encompass various aspects, ranging from the understanding of its anatomy and function to the diagnosis, treatment options, prognosis, and prevention of disorders related to this vital nerve.
Understanding the Accessory Nerve
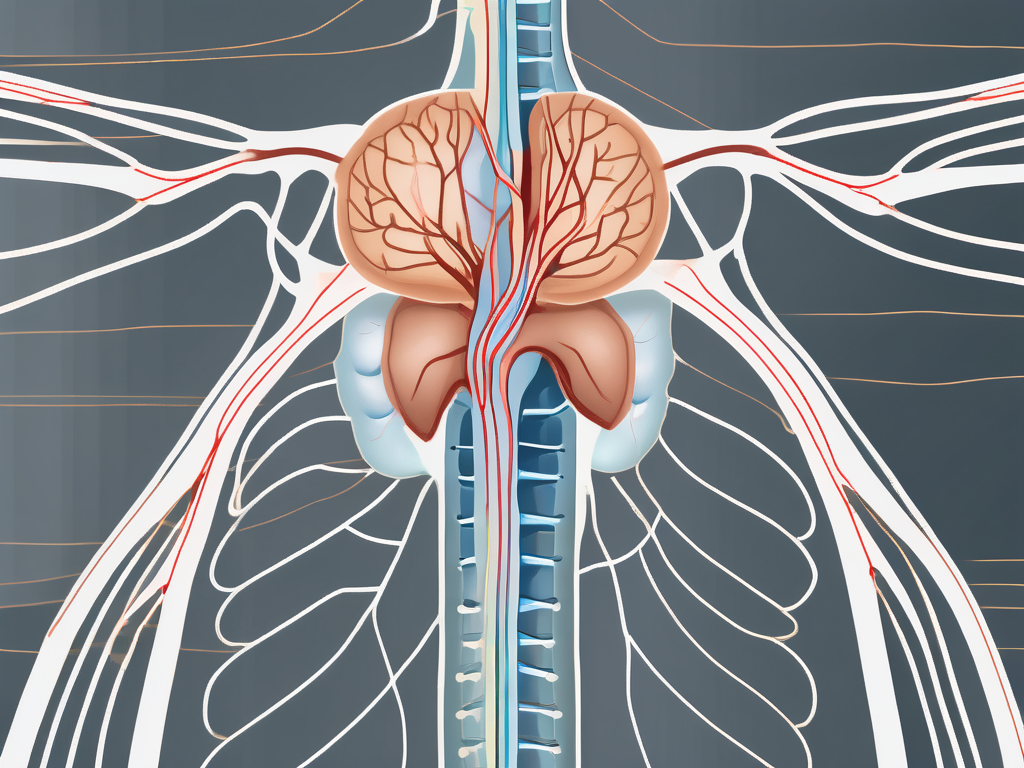
The accessory nerve, also known as cranial nerve XI, is a complex motor nerve that originates in the brainstem and extends to the neck and upper back. It consists of two components: the cranial part, which arises from the motor nuclei of the medulla oblongata, and the spinal part, which emerges from the upper cervical spinal cord.
The cranial part of the accessory nerve joins with the vagus nerve to innervate the muscles responsible for swallowing and phonation. This intricate connection allows for the precise coordination of movements involved in these vital functions. When we swallow, the accessory nerve works in conjunction with the vagus nerve to contract the muscles of the throat, ensuring the smooth passage of food and liquids. Similarly, during phonation, the accessory nerve helps control the muscles involved in speech production, allowing us to articulate sounds and communicate effectively.
On the other hand, the spinal part of the accessory nerve supplies the trapezius and sternocleidomastoid muscles, contributing to head and shoulder movements. The trapezius muscle, located in the upper back and neck, plays a crucial role in stabilizing and moving the shoulder blades. It allows us to perform actions such as shrugging our shoulders and pulling them back. The sternocleidomastoid muscle, found in the front of the neck, enables us to rotate and tilt our heads. It is responsible for movements like turning our heads from side to side and looking up or down.
The accessory nerve’s function is not limited to individual muscle movements; it also plays a significant role in overall neck stability. By coordinating the actions of various neck and shoulder muscles, the accessory nerve helps maintain proper alignment and support for the head and neck. This stability is crucial for everyday activities such as maintaining an upright posture, holding our heads steady, and engaging in physical tasks that involve the neck and shoulders.
In summary, the accessory nerve is a multifaceted cranial nerve that serves essential functions in the body. From enabling the precise coordination of swallowing and phonation to facilitating head and shoulder movements and maintaining neck stability, this nerve plays a vital role in our everyday lives.
Clinical Presentations of Accessory Nerve Disorders
Symptoms of Accessory Nerve Damage
When the accessory nerve is impaired or damaged, it can lead to a variety of symptoms. These may include weakness or atrophy of the trapezius and sternocleidomastoid muscles, resulting in difficulties in shoulder movements, head rotation, and raising the arms.
Additionally, individuals with accessory nerve disorders may experience pain and tenderness in the affected muscles, neck stiffness, and difficulty in performing tasks that require upper body strength, such as lifting objects or participating in sports activities.
Moreover, the impact of accessory nerve damage goes beyond physical limitations. Patients often report feelings of frustration, as their ability to engage in daily activities and hobbies becomes compromised. The loss of independence and the need for assistance can lead to emotional distress and a decrease in overall quality of life.
It is important to note that these symptoms can vary in severity, and consultation with a healthcare professional is necessary to identify and address the specific issues at hand. A thorough evaluation, including a physical examination and possibly diagnostic tests, is crucial for an accurate diagnosis and appropriate management of accessory nerve disorders.
Causes of Accessory Nerve Disorders
Accessory nerve disorders can occur due to various factors, including traumatic injuries, such as neck trauma or surgical procedures involving the neck or shoulder area. Inflammatory conditions, infections, and tumors affecting the nerve can also lead to disorders.
Furthermore, certain medical conditions, such as nerve entrapment syndromes or autoimmune diseases, may contribute to the development of accessory nerve disorders. Identifying the underlying cause is crucial for determining an appropriate treatment plan.
It is worth mentioning that prevention plays a significant role in reducing the risk of accessory nerve disorders. Taking precautions to avoid traumatic injuries, such as wearing protective gear during sports activities or practicing proper body mechanics during physical tasks, can help minimize the likelihood of nerve damage. Additionally, maintaining a healthy lifestyle, including regular exercise and a balanced diet, can contribute to overall nerve health and reduce the risk of developing nerve-related disorders.
When it comes to treatment, the approach depends on the underlying cause and the severity of the symptoms. Conservative management options, such as physical therapy, pain management techniques, and lifestyle modifications, are often recommended as initial steps. In more severe cases, surgical interventions may be necessary to repair or reconstruct the damaged nerve.
Overall, early recognition and prompt intervention are essential in managing accessory nerve disorders effectively. Seeking medical attention at the first sign of symptoms can help prevent further damage and improve the chances of successful treatment outcomes.
Diagnostic Procedures for Accessory Nerve Disorders
When it comes to diagnosing accessory nerve disorders, physical examination is a crucial step. A skilled healthcare professional will carefully assess various aspects of the patient’s neck and shoulder area. They will evaluate the range of motion, muscle strength, and symmetry in these regions. To further evaluate the function of specific muscles like the trapezius and sternocleidomastoid, they may perform tests such as the shoulder shrug and head turn tests.
However, physical examination is not the only tool used in diagnosing accessory nerve disorders. Gathering a comprehensive medical history and conducting detailed discussions with the patient are equally important. These steps help identify potential causes and rule out other conditions that may mimic the symptoms of accessory nerve disorders.
Imaging Techniques
In addition to physical examination and patient interviews, healthcare professionals may employ various imaging techniques to aid in the diagnosis of accessory nerve disorders. Magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly used to visualize the structures, nerves, and surrounding tissues in the neck and shoulder area. These imaging techniques can help detect any abnormalities or injuries that may be affecting the accessory nerve.
Electromyography and Nerve Conduction Studies
In certain cases, electromyography (EMG) and nerve conduction studies (NCS) may be conducted to further evaluate the nerve function and identify the specific site or extent of the damage. EMG involves the insertion of small needles into the muscles to measure their electrical activity. NCS, on the other hand, measures the speed and strength of electrical signals as they travel along the nerves. These tests can provide valuable information about the health and functionality of the accessory nerve.
By utilizing a combination of physical examination, medical history, imaging techniques, and specialized tests like EMG and NCS, healthcare professionals can accurately diagnose accessory nerve disorders. This comprehensive approach ensures that patients receive the appropriate treatment and care for their specific condition.
Treatment Options for Accessory Nerve Disorders
The accessory nerve, also known as the 11th cranial nerve, plays a vital role in controlling certain muscles in the head, neck, and shoulders. When this nerve becomes damaged or dysfunctional, it can lead to a variety of symptoms and impairments. Fortunately, there are several treatment options available to address accessory nerve disorders.
Non-Surgical Treatments
Non-surgical approaches are usually the first line of treatment for accessory nerve disorders. These may include physical therapy sessions focused on muscle strengthening and range of motion exercises to improve functionality.
During physical therapy sessions, patients work closely with trained professionals who guide them through specific exercises designed to target the affected muscles. These exercises not only help strengthen the muscles but also enhance their coordination and flexibility.
In addition to physical therapy, pain management techniques can play a crucial role in alleviating discomfort associated with accessory nerve disorders. Nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants may be prescribed to reduce inflammation and relieve pain.
Alternative therapies, such as acupuncture or transcutaneous electrical nerve stimulation (TENS), may also provide some relief for certain individuals. Acupuncture involves the insertion of thin needles into specific points on the body to stimulate the nervous system and promote healing. TENS, on the other hand, uses low-voltage electrical currents to target and stimulate the affected nerves.
It is crucial to note that the treatment plan for accessory nerve disorders will depend on various factors, including the underlying cause, severity of symptoms, and individual patient factors. Therefore, a consultation with a healthcare professional is essential for personalized guidance and to determine the most appropriate non-surgical treatments.
Surgical Interventions
In cases where non-surgical treatments fail to provide significant improvement or when there is structural damage to the accessory nerve, surgical interventions may be considered. The specific surgical approach will depend on the identified cause and location of the problem.
Nerve repair is a common surgical procedure for accessory nerve disorders. During this procedure, the damaged portion of the nerve is carefully identified and repaired, allowing for improved nerve function. In some cases, nerve grafts may be necessary to bridge the gap between damaged nerve segments and promote nerve regeneration.
Another surgical option is decompression, which involves relieving any nerve entrapment that may be causing the accessory nerve disorder. By removing or repositioning the structures compressing the nerve, surgeons can help restore proper nerve function and alleviate symptoms.
Rehabilitation following surgery is often crucial to regain optimal muscle function and promote recovery. This may involve a combination of physical therapy, occupational therapy, and speech therapy, depending on the specific impairments caused by the accessory nerve disorder.
In conclusion, treatment options for accessory nerve disorders range from non-surgical approaches, such as physical therapy and pain management techniques, to surgical interventions like nerve repair or decompression. The choice of treatment depends on various factors and should be discussed with a healthcare professional to ensure the most effective and personalized approach for each individual.
Prognosis and Recovery from Accessory Nerve Disorders
Accessory nerve disorders can have varying prognoses depending on several factors. These factors include the cause of the disorder, the extent of damage to the nerve, and individual characteristics of the patient. Early diagnosis and prompt initiation of appropriate treatment can significantly enhance the chances of recovery.
In addition to the aforementioned factors, the patient’s overall health and adherence to rehabilitation protocols can also play a key role in the recovery process. It is important for patients to establish realistic expectations and work closely with healthcare professionals to support the best possible outcome.
Rehabilitation programs, such as physical therapy and occupational therapy, are fundamental components of the recovery process for accessory nerve disorders. These programs aim to restore muscle strength, improve range of motion, and enhance functional abilities.
Physical therapy focuses on exercises and techniques that help strengthen the affected muscles and improve coordination. This may involve various exercises, such as stretching, resistance training, and balance exercises. The therapist may also use modalities like heat or cold therapy, electrical stimulation, or ultrasound to aid in the recovery process.
Occupational therapy, on the other hand, focuses on helping patients regain their ability to perform daily activities and tasks. This may involve techniques to improve fine motor skills, coordination, and dexterity. The therapist may also provide adaptive devices or assistive technology to aid in the recovery process.
Recovery timelines can vary significantly depending on the severity of the disorder and the individual’s response to treatment. It is crucial for patients to follow the guidance of healthcare professionals and engage in regular follow-up visits to monitor progress and ensure appropriate adjustments to the treatment plan.
During the recovery process, it is common for patients to experience ups and downs. Some days may show more progress, while others may be more challenging. It is important for patients to stay motivated and committed to their rehabilitation program, as consistency and perseverance are key to achieving optimal recovery.
In addition to physical and occupational therapy, lifestyle modifications can also play a significant role in the recovery process. This may include adopting a healthy diet, managing stress levels, and incorporating regular exercise into daily routines. These lifestyle modifications can support overall health and well-being, which can positively impact the recovery from accessory nerve disorders.
In conclusion, the prognosis and recovery from accessory nerve disorders depend on various factors, including the cause, extent of damage, and individual characteristics. Rehabilitation programs, such as physical therapy and occupational therapy, are crucial in the recovery process. Patients should work closely with healthcare professionals, follow treatment plans, and make lifestyle modifications to support the best possible outcome.
Prevention and Management of Accessory Nerve Disorders
Lifestyle Modifications
To reduce the risk of accessory nerve disorders or prevent their recurrence, certain lifestyle modifications may be beneficial. Maintaining proper posture, engaging in regular exercise, and avoiding repetitive movements or excessive strain on the neck and shoulder region are important precautions.
Proper posture is crucial for the health of the accessory nerve. When we slouch or hunch our shoulders forward, it can put unnecessary pressure on the nerve, leading to discomfort and potential disorders. By consciously maintaining an upright posture, with our shoulders relaxed and our spine aligned, we can help alleviate this pressure and promote optimal nerve function.
In addition to posture, regular exercise plays a significant role in preventing accessory nerve disorders. Engaging in activities that strengthen the neck and shoulder muscles, such as yoga or weightlifting, can help improve the overall stability and support of the nerve. It is important, however, to avoid overexertion or excessive strain on these muscles, as it can lead to unnecessary stress on the accessory nerve.
Ergonomic adjustments in the workplace or during daily activities can also contribute to the prevention of accessory nerve disorders. Using supportive pillows that provide adequate neck and shoulder support, as well as ensuring comfortable seating positions, can help minimize stress on these muscles. Additionally, taking regular breaks to stretch and relax the neck and shoulder region can further alleviate any tension that may accumulate throughout the day.
Regular Check-ups and Monitoring
Regular check-ups with a healthcare professional are essential, particularly for individuals with a history of accessory nerve disorders or those experiencing persistent symptoms. These check-ups allow for early detection of any changes in nerve function and facilitate timely intervention if necessary.
During these check-ups, healthcare professionals may perform various tests to assess the health of the accessory nerve. These tests can include electromyography (EMG), which measures the electrical activity of the muscles, and nerve conduction studies, which evaluate the speed and strength of nerve signals. By monitoring the progress of the accessory nerve and identifying any abnormalities, healthcare professionals can provide appropriate treatment and management strategies tailored to the individual’s needs.
Furthermore, regular check-ups also provide an opportunity to manage any underlying conditions that may contribute to accessory nerve disorders. Conditions such as cervical spine abnormalities, tumors, or infections can affect the health of the nerve and may require specific interventions. By addressing these underlying conditions, healthcare professionals can help individuals maintain optimal nerve health and overall well-being.
In conclusion, understanding the clinical presentations of the accessory nerve involves gaining insight into its anatomy, function, and associated disorders. Timely diagnosis, appropriate treatment, diligent rehabilitation, and proactive prevention measures are vital in managing accessory nerve disorders and promoting recovery. Remember, if you suspect any issues related to the accessory nerve, consult with a qualified healthcare professional for comprehensive evaluation and guidance tailored to your specific needs.


