what doctor to see for spinal accessory nerve injury
Spinal accessory nerve injury can be a concerning condition that may require specialized medical attention. Understanding the causes, symptoms, and treatment options associated with this type of injury is essential for proper diagnosis and management. In this article, we will explore the role of different medical specialists in addressing spinal accessory nerve injury, the available treatment options, the recovery and rehabilitation process, as well as prevention and long-term management strategies.
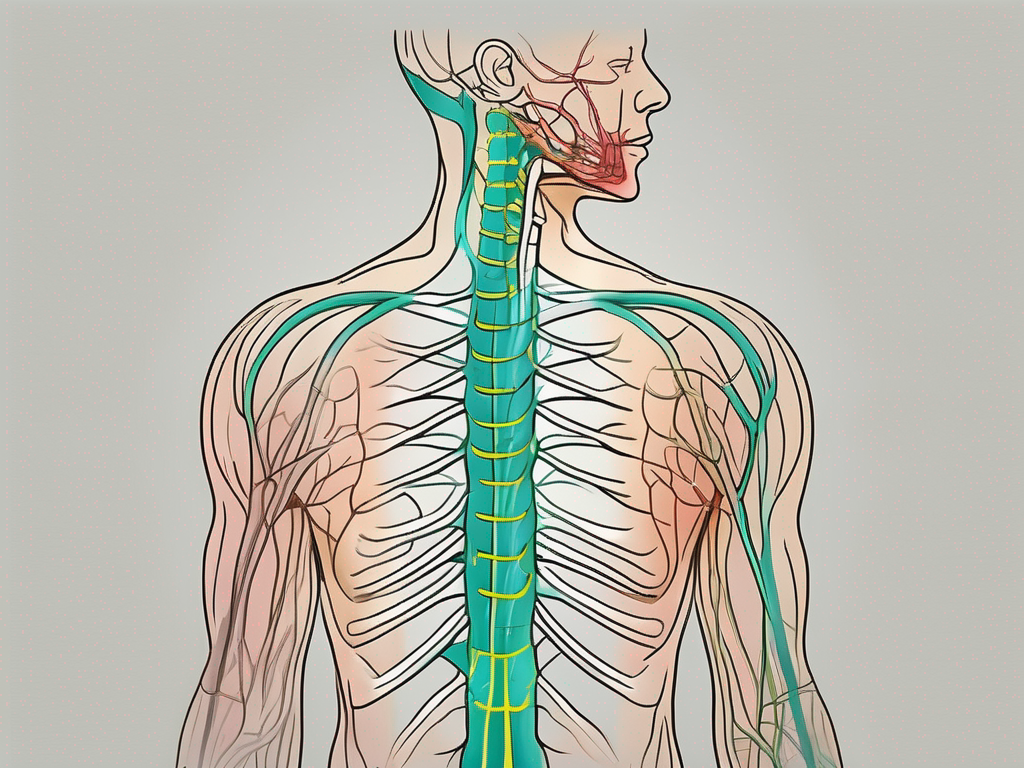
Understanding Spinal Accessory Nerve Injury
Spinal accessory nerve injury, also known as accessory nerve palsy, is a condition that affects the nerves responsible for controlling certain muscles in the neck and shoulders. This can result from trauma, such as motor vehicle accidents, sports injuries, or surgical procedures in the neck and shoulder area. It may also be associated with underlying medical conditions, such as tumors or infections.
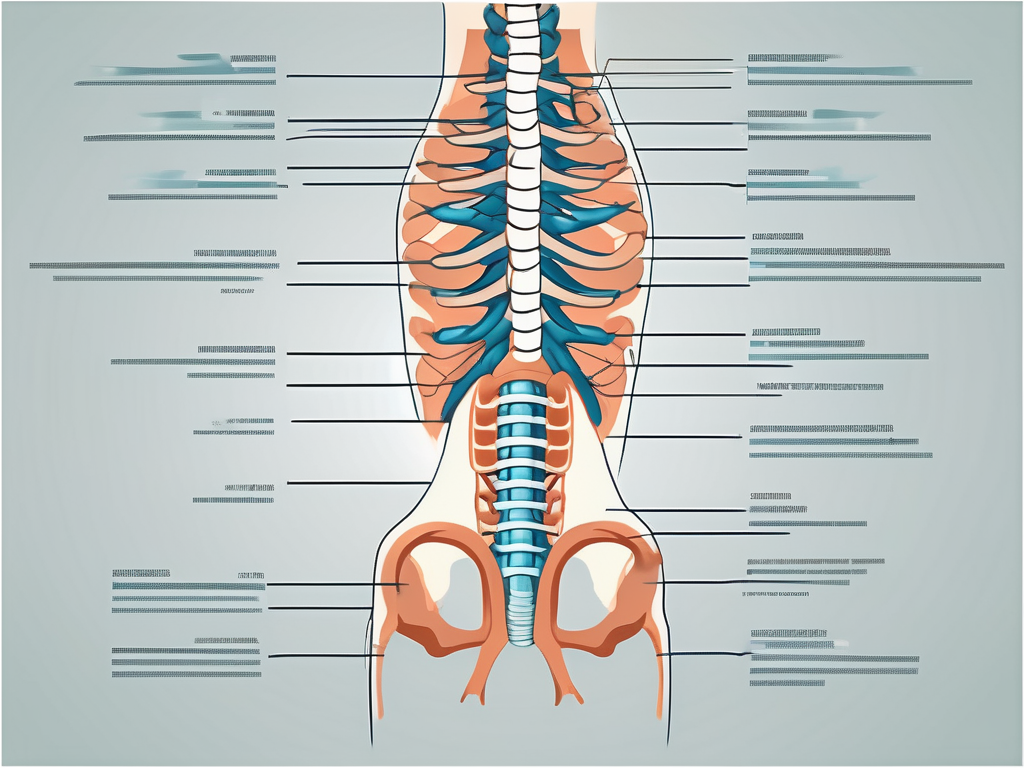
The spinal accessory nerve, also known as cranial nerve XI, is a motor nerve that originates in the brainstem and travels down the neck to innervate the trapezius and sternocleidomastoid muscles. These muscles are important for various movements of the head, neck, and shoulders, including rotation, flexion, and extension. When the spinal accessory nerve is injured, it can lead to weakness or paralysis of these muscles, resulting in functional limitations and discomfort.
Causes of Spinal Accessory Nerve Injury
The spinal accessory nerve can be damaged by direct trauma, stretching, or compression. Injuries to the neck and shoulder region, such as whiplash, can contribute to nerve damage. The sudden and forceful movement of the head and neck in a car accident or during sports activities can put strain on the nerve, leading to injury. Additionally, surgeries involving the neck or shoulder area, such as lymph node removal or neck dissection, may also lead to nerve injury. These procedures often require careful dissection and manipulation of tissues, which can inadvertently damage the spinal accessory nerve.
Furthermore, certain medical conditions can also contribute to spinal accessory nerve injury. Tumors in the neck or shoulder region can exert pressure on the nerve, causing damage. Infections, such as viral or bacterial infections, can also affect the nerve’s function. It is important for healthcare professionals to consider these underlying causes when evaluating and managing patients with spinal accessory nerve injury.
Symptoms and Diagnosis of Spinal Accessory Nerve Injury
Common symptoms of spinal accessory nerve injury include weakness or paralysis of specific muscles in the neck and shoulders, difficulty lifting the arm, and pain or discomfort in the affected area. The trapezius muscle, which is innervated by the spinal accessory nerve, plays a crucial role in shoulder movement and stability. When this muscle is weakened or paralyzed, it can lead to difficulty in raising the arm above the shoulder level or maintaining proper posture.
In addition to muscle weakness, individuals with spinal accessory nerve injury may experience numbness or tingling sensations in the affected area. This can be due to altered sensory input from the damaged nerve fibers. The combination of motor and sensory symptoms can significantly impact a person’s quality of life and daily activities.
Diagnosing spinal accessory nerve injury involves a comprehensive evaluation by a healthcare professional. A thorough medical history, including information about any recent trauma, surgeries, or underlying medical conditions, is essential. A physical examination will assess muscle strength, range of motion, and any signs of atrophy or muscle wasting. Diagnostic tests, such as electromyography (EMG) and nerve conduction studies, may also be performed to evaluate the function of the spinal accessory nerve and confirm the diagnosis.
The Role of Different Medical Specialists
Addressing spinal accessory nerve injury often requires a multidisciplinary approach involving various medical specialists. While the primary care physician plays a crucial role in the initial assessment and referral, several specialists may be involved in the comprehensive management of this condition.
The Neurologist’s Perspective
A neurologist specializes in diagnosing and treating conditions that affect the nervous system, including nerve injuries. They may perform neurological examinations, order further diagnostic tests, and recommend appropriate treatment options. Neurologists can help evaluate the extent of nerve damage and guide the overall management plan.
When a patient with spinal accessory nerve injury visits a neurologist, the specialist will conduct a thorough assessment to understand the specific symptoms and challenges faced by the individual. This may involve testing the patient’s muscle strength, coordination, and reflexes. The neurologist will also review the patient’s medical history and any previous diagnostic tests to gain a comprehensive understanding of the condition.
Based on the assessment, the neurologist may order additional tests such as electromyography (EMG) or nerve conduction studies to evaluate the function and integrity of the spinal accessory nerve. These tests can provide valuable information about the severity and location of the nerve injury, helping the neurologist determine the most appropriate treatment approach.
Once a diagnosis is made, the neurologist will discuss the available treatment options with the patient. This may include non-surgical interventions such as physical therapy, medication management, or lifestyle modifications. In cases where surgical intervention is necessary, the neurologist will coordinate with other specialists, such as orthopedic surgeons, to ensure a comprehensive and coordinated approach to care.
The Role of an Orthopedic Surgeon
Orthopedic surgeons have expertise in treating musculoskeletal conditions, including nerve injuries. In cases of severe nerve damage or when surgical intervention is necessary, an orthopedic surgeon may perform specialized procedures to repair or graft the damaged nerve. They can also provide guidance on postoperative care and rehabilitation.
When a patient with spinal accessory nerve injury requires surgical intervention, the orthopedic surgeon will carefully evaluate the extent of the nerve damage and determine the most appropriate surgical approach. This may involve techniques such as nerve grafting, where a healthy nerve is used to bridge the gap between the damaged nerve ends, or nerve transfer, where a nearby functioning nerve is redirected to restore function.
Following surgery, the orthopedic surgeon will closely monitor the patient’s progress and provide guidance on postoperative care. This may include recommendations for physical therapy, pain management, and the use of assistive devices to aid in daily activities. The surgeon will work in collaboration with other specialists, such as physical therapists, to ensure a comprehensive and coordinated approach to rehabilitation.
When to Consult a Physical Therapist
Physical therapists play a vital role in the recovery and rehabilitation process for spinal accessory nerve injury. They can design and implement specific exercise programs aimed at restoring muscle strength, improving flexibility, and facilitating functional recovery. Physical therapists can also provide guidance on pain management techniques and assistive devices that may aid in daily activities.
When a patient with spinal accessory nerve injury begins physical therapy, the therapist will conduct a comprehensive evaluation to assess the individual’s physical abilities and limitations. This may involve assessing muscle strength, range of motion, coordination, and balance. The therapist will also take into consideration the patient’s goals and expectations for recovery.
Based on the evaluation, the physical therapist will develop a personalized treatment plan tailored to the patient’s specific needs. This may include a combination of therapeutic exercises, manual therapy techniques, and modalities such as electrical stimulation or ultrasound. The therapist will closely monitor the patient’s progress and make adjustments to the treatment plan as needed.
Physical therapists also play a crucial role in educating patients about self-care strategies and techniques to manage pain and prevent further injury. They can provide guidance on proper body mechanics, ergonomic modifications, and the use of assistive devices to support daily activities. Through regular physical therapy sessions, patients can gradually regain strength, improve mobility, and enhance their overall quality of life.
Treatment Options for Spinal Accessory Nerve Injury
The spinal accessory nerve plays a crucial role in controlling the movement of certain muscles in the neck and shoulder. When this nerve is injured, it can lead to a range of symptoms and functional limitations. The choice of treatment for spinal accessory nerve injury depends on the severity of the injury, the underlying cause, and individual patient factors.
When it comes to treating spinal accessory nerve injuries, there are two main categories of treatment options: surgical interventions and non-surgical treatments. The decision on which approach to take is based on a thorough evaluation of the patient’s condition and the recommendations of a specialist, such as an orthopedic surgeon.
Surgical Interventions
In cases of severe nerve damage or when conservative measures fail to provide adequate improvement, surgical interventions may be considered. These procedures aim to repair or restore the damaged nerve, allowing for improved function and symptom relief.
One surgical option for spinal accessory nerve injury is nerve repair. This involves reconnecting the damaged nerve ends to promote nerve regeneration and restore proper function. Nerve repair is typically performed using microsurgical techniques, which allow for precise alignment of the nerve ends.
In cases where the nerve damage is more extensive, nerve grafting may be necessary. This procedure involves taking a healthy nerve from another part of the body and using it to bridge the gap between the damaged nerve ends. This allows for the regeneration of the damaged nerve over time.
Another surgical approach that may be considered is nerve transfer. This involves transferring a healthy nerve from a different muscle or nerve group to the affected area. The transferred nerve then takes over the function of the damaged spinal accessory nerve, restoring movement and function.
It is important to note that the choice of surgical intervention depends on various factors, including the extent of the nerve injury, the patient’s overall health, and the surgeon’s expertise. A thorough evaluation and consultation with a specialist are essential to determine the most appropriate surgical approach.
Non-Surgical Treatments
Non-surgical treatments for spinal accessory nerve injury are typically aimed at managing symptoms, promoting functional recovery, and improving the patient’s quality of life. These treatments may be recommended as the first line of treatment or in cases where surgery is not feasible or necessary.
Physical therapy is a key component of non-surgical treatment for spinal accessory nerve injury. A skilled physical therapist can design a customized rehabilitation program that focuses on strengthening the muscles affected by the nerve injury, improving range of motion, and enhancing overall function. Physical therapy may include exercises, manual therapy techniques, and modalities such as heat or cold therapy.
Pain management techniques may also be utilized to help alleviate discomfort associated with spinal accessory nerve injury. This may include the use of medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or nerve pain medications, as well as alternative therapies like acupuncture or transcutaneous electrical nerve stimulation (TENS).
In some cases, the use of assistive devices, such as braces or slings, may be recommended to provide support and stability to the affected area. These devices can help reduce strain on the muscles and allow for better healing and recovery.
A multi-modal approach that combines various non-surgical treatments may be recommended to optimize the recovery process. This may involve a combination of physical therapy, pain management techniques, and the use of assistive devices, tailored to the individual needs of the patient.
In conclusion, the treatment options for spinal accessory nerve injury are diverse and depend on the severity of the injury, the underlying cause, and individual patient factors. Surgical interventions, such as nerve repair, nerve grafting, or nerve transfer, may be considered in severe cases or when conservative measures fail. Non-surgical treatments, including physical therapy, pain management techniques, and the use of assistive devices, can also play a crucial role in managing symptoms and promoting functional recovery. It is important to consult with a specialist to determine the most appropriate treatment approach for each individual case.
Recovery and Rehabilitation Process
The recovery and rehabilitation process for spinal accessory nerve injury can vary depending on the severity of the injury and individual patient factors. It is important to set realistic goals and work closely with healthcare professionals to optimize the recovery process.
When it comes to recovering from a spinal accessory nerve injury, patience and perseverance are key. The journey to full recovery can be challenging, but with the right approach and guidance, it is possible to regain strength and function.
One important aspect of the recovery process is understanding the expected timeline. While every individual is unique and may experience different rates of recovery, there are general guidelines to consider. In mild cases, spontaneous recovery may occur within a few weeks to months. This means that with time, the nerve may heal itself and gradually restore its normal function.
However, for more severe injuries, the recovery timeline may be longer. It is not uncommon for individuals with significant nerve damage to require a more extended period of rehabilitation. In these cases, consistent follow-up with healthcare professionals is essential to monitor progress and make necessary adjustments to the rehabilitation plan.
Expected Recovery Timeline
The recovery timeline for spinal accessory nerve injury can vary significantly from individual to individual. While some may experience a faster recovery, others may need more time and patience. It is important to remember that each person’s journey is unique, and comparing oneself to others may not be helpful.
During the recovery process, it is crucial to stay positive and focus on small victories. Celebrating even the smallest improvements can provide motivation and encouragement to keep pushing forward.
Rehabilitation Exercises and Therapies
Physical therapy plays a crucial role in the rehabilitation process for spinal accessory nerve injury. Under the guidance of a skilled physical therapist, individuals can engage in specific exercises and therapies to aid in their recovery.
Rehabilitation exercises and therapies aim to restore muscle strength, improve range of motion, and enhance functional abilities. The physical therapist will design a personalized exercise program tailored to the individual’s needs and goals.
These exercises may include stretching, strengthening, and coordination exercises. Stretching exercises help improve flexibility and prevent muscle tightness, while strengthening exercises target the affected muscles and surrounding areas to rebuild strength. Coordination exercises focus on improving the coordination between the nerves and muscles, facilitating optimal movement.
In addition to physical therapy, other complementary therapies may be beneficial in the recovery process. These may include occupational therapy, massage therapy, and acupuncture. These therapies can help address specific challenges and promote overall well-being.
It is important to note that the recovery and rehabilitation process is not a linear journey. There may be setbacks along the way, but with determination and the support of healthcare professionals, individuals can overcome these obstacles and continue moving forward.
Remember, the road to recovery may be long, but with perseverance and a comprehensive rehabilitation plan, individuals can regain their strength, function, and independence.
Prevention and Management of Future Injuries
While not all spinal accessory nerve injuries are preventable, certain lifestyle changes and strategies can help reduce the risk of future injuries or exacerbation of existing conditions.
Lifestyle Changes for Prevention
Avoiding activities that may pose a risk of traumatic injury to the neck and shoulders, such as participating in contact sports without appropriate protective gear, can help reduce the likelihood of spinal accessory nerve injury. Maintaining proper posture and using correct lifting techniques can also minimize the risk of nerve damage.
Long-Term Management Strategies
For individuals with persistent symptoms or long-term impairments, implementing long-term management strategies is essential for maintaining functional abilities and optimizing quality of life. This may involve ongoing physical therapy, pain management techniques, and assistive devices as needed. Regular follow-up with healthcare professionals can ensure that any changes in symptoms or functional abilities are promptly addressed.
In conclusion, spinal accessory nerve injury requires careful evaluation and management by medical specialists with experience in this area. By understanding the causes, symptoms, and treatment options associated with this type of injury, individuals can seek appropriate medical attention and improve their chances of recovery. An inter-disciplinary approach involving neurologists, orthopedic surgeons, and physical therapists can help optimize the overall management plan. Additionally, a focus on prevention and long-term management strategies can reduce the risk of future injuries and enhance quality of life. If you suspect a spinal accessory nerve injury, it is crucial to consult with a doctor for a comprehensive evaluation and personalized treatment plan.