what is accessory nerve palsy
The accessory nerve is an important component of the human nervous system. It plays a crucial role in facilitating the movement of various muscles involved in head and neck actions. When this nerve is affected by palsy, it can lead to a condition known as accessory nerve palsy.
Understanding the Accessory Nerve
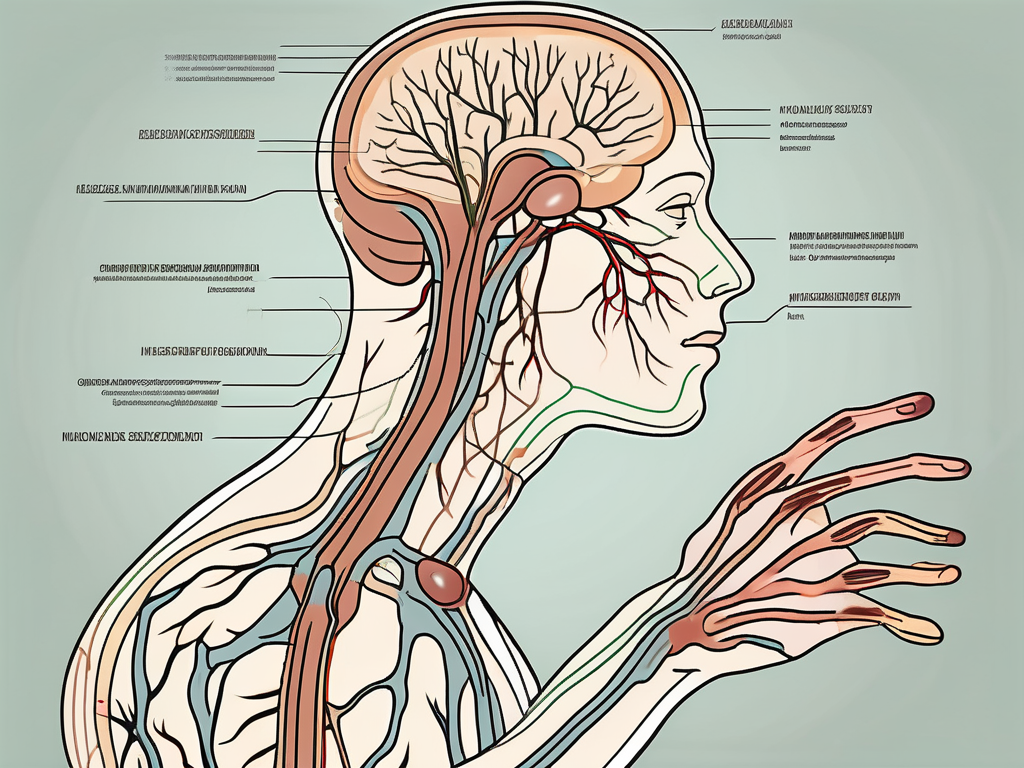
Before delving into the various aspects of accessory nerve palsy, it is important to gain a clear understanding of the nerve itself. The accessory nerve, also known as cranial nerve XI, is a motor nerve that originates from the brainstem and travels down the neck.
Anatomy of the Accessory Nerve
The accessory nerve consists of two main components: the cranial component and the spinal component. The cranial component arises from the brainstem, while the spinal component emerges from the upper spinal cord regions. These two components come together to form a single nerve that supplies various muscles in the head and neck.
The cranial component of the accessory nerve begins its journey from the lateral aspect of the medulla oblongata, a vital part of the brainstem responsible for controlling many involuntary functions. It then traverses through the jugular foramen, a small opening in the base of the skull, to join the spinal component.
The spinal component of the accessory nerve arises from the upper spinal cord regions, specifically from the anterior horn cells of the upper cervical spinal cord segments. It exits the spinal cord through the ventral root and joins the cranial component in the jugular foramen.
Once the cranial and spinal components unite, the accessory nerve continues its course downward, passing through the neck alongside other important structures such as the internal jugular vein and the carotid artery. It then branches out to innervate various muscles in the head and neck region.
Function of the Accessory Nerve
The primary function of the accessory nerve is to control the movement of specific muscles involved in head and neck actions. It innervates muscles such as the sternocleidomastoid and trapezius, which contribute to head rotation, shoulder movement, and overall posture.
The sternocleidomastoid muscle, innervated by the accessory nerve, plays a crucial role in tilting and rotating the head. It originates from the sternum and clavicle and inserts into the mastoid process of the temporal bone. When both sternocleidomastoid muscles contract together, they flex the neck forward. However, when only one muscle contracts, it causes rotation of the head to the opposite side.
The trapezius muscle, also innervated by the accessory nerve, is responsible for various movements of the shoulder girdle. It extends from the base of the skull and the cervical and thoracic vertebrae to the spine of the scapula and the acromion process of the scapula. Contraction of the trapezius muscle allows for elevation, retraction, and rotation of the scapula, contributing to movements such as shrugging the shoulders and pulling them back.
In addition to its role in head and neck movements, the accessory nerve also plays a role in maintaining proper posture. The coordinated action of the sternocleidomastoid and trapezius muscles, under the control of the accessory nerve, helps to stabilize the head, neck, and shoulders, allowing for efficient and balanced movement.
Understanding the anatomy and function of the accessory nerve is essential in comprehending the various conditions and disorders that can affect its normal functioning. By gaining a thorough knowledge of this important cranial nerve, healthcare professionals can better diagnose and treat patients with accessory nerve-related issues.
The Nature of Nerve Palsy
Nerve palsy, including accessory nerve palsy, refers to the impairment or loss of normal nerve function. It can be caused by various factors, such as physical trauma, infections, or underlying medical conditions. This condition affects the normal functioning of the nerve, leading to a range of symptoms.
Nerve palsy is a complex condition that can have a significant impact on an individual’s daily life. The affected nerve plays a crucial role in transmitting signals from the brain to the muscles, allowing for coordinated movement and sensation. When the nerve is damaged or impaired, these signals are disrupted, resulting in a variety of symptoms.
General Overview of Nerve Palsy
Nerve palsy can manifest differently depending on the affected nerve and its function. Common symptoms include muscle weakness, loss of sensation, and coordination difficulties. In the case of accessory nerve palsy, individuals may experience difficulty in moving their head, neck, and shoulders.
Imagine waking up one day and finding it difficult to move your head or shoulders. Simple tasks like turning your head to check for oncoming traffic or lifting your arm to reach for something become challenging and frustrating. This is the reality for individuals with accessory nerve palsy.
Accessory nerve palsy specifically affects the accessory nerve, also known as the eleventh cranial nerve. This nerve is responsible for controlling the movement of certain muscles in the head, neck, and shoulders. When the nerve is damaged or compressed, as is the case with palsy, these muscles are unable to function properly, leading to limited movement and discomfort.
Causes and Risk Factors of Nerve Palsy
Accessory nerve palsy can have multiple causes and risk factors. Physical trauma, such as neck injuries or surgery, can lead to nerve damage and subsequent palsy. Other potential causes include viral infections, tumors, or autoimmune disorders. Risk factors may include participation in contact sports, occupations demanding repetitive neck movements, or underlying medical conditions.
One of the most common causes of accessory nerve palsy is physical trauma. This can occur as a result of a car accident, sports injury, or even a fall. The forceful impact on the head or neck can cause the accessory nerve to become damaged, leading to palsy. In some cases, surgical procedures that involve the neck area can also inadvertently damage the nerve, resulting in palsy.
Infections, such as viral infections, can also contribute to the development of accessory nerve palsy. Viruses can attack and inflame the nerve, disrupting its normal function. Additionally, certain tumors or growths in the neck region can put pressure on the accessory nerve, causing it to malfunction.
Occupations or activities that require repetitive neck movements can increase the risk of developing accessory nerve palsy. People who work in professions that involve constant head and neck movements, such as construction workers or professional athletes, may be more susceptible to nerve damage. Furthermore, individuals with underlying medical conditions, such as autoimmune disorders, may have a higher risk of developing nerve palsy.
Understanding the causes and risk factors of accessory nerve palsy is crucial in both prevention and treatment. By identifying and addressing these factors, healthcare professionals can work towards minimizing the occurrence of this debilitating condition.
Delving into Accessory Nerve Palsy
Accessory nerve palsy is a specific condition that requires focused examination. Understanding its symptoms and causes is essential for proper diagnosis and management.
Accessory nerve palsy, also known as cranial nerve XI palsy, is a condition that affects the function of the accessory nerve, which is responsible for controlling certain muscles in the head and neck. This condition can have a significant impact on a person’s daily life, as it can lead to difficulties in performing basic movements and activities.
Symptoms of Accessory Nerve Palsy
The primary symptoms of accessory nerve palsy revolve around difficulties in head and neck movements. Individuals may experience weakness or inability to rotate their head or move their shoulders properly. This can make simple tasks like turning to look at something or lifting objects challenging and frustrating.
In addition to the movement difficulties, individuals with accessory nerve palsy may also notice pain or discomfort in the neck or shoulder regions. This pain can range from mild to severe and may be accompanied by muscle stiffness or tightness. The pain can further limit the range of motion and affect the overall quality of life.
In severe cases of accessory nerve palsy, muscle atrophy or wasting may become visible. This occurs when the affected muscles start to shrink and lose their strength due to lack of use. Muscle atrophy can further exacerbate the movement difficulties and lead to additional complications.
Causes of Accessory Nerve Palsy
Accessory nerve palsy can arise from various factors. Physical trauma, such as car accidents or sports injuries, is a common cause. The sudden impact or force can damage the accessory nerve, leading to its dysfunction. It is crucial to seek immediate medical attention after any head or neck injury to prevent further complications.
Additionally, surgical procedures involving the neck or shoulders can result in nerve damage and subsequent accessory nerve palsy. While surgical interventions are often necessary for various medical conditions, it is essential to discuss the potential risks and complications with the healthcare provider beforehand.
In some cases, infections, tumors, or autoimmune disorders may contribute to the development of accessory nerve palsy. Infections, such as viral or bacterial meningitis, can cause inflammation and damage to the accessory nerve. Tumors or growths in the head or neck region can also put pressure on the nerve, leading to its dysfunction. Autoimmune disorders, where the immune system mistakenly attacks the body’s own tissues, can also affect the accessory nerve.
Proper diagnosis of the underlying cause of accessory nerve palsy is crucial for effective management and treatment. Medical professionals may perform various tests, such as physical examinations, imaging studies, or nerve conduction studies, to determine the cause and extent of the nerve damage.
In conclusion, accessory nerve palsy is a condition that can significantly impact a person’s ability to perform basic head and neck movements. Understanding the symptoms and causes of this condition is essential for proper diagnosis and management. If you or someone you know is experiencing difficulties in head and neck movements, it is important to seek medical attention for a thorough evaluation and appropriate treatment.
Diagnosing Accessory Nerve Palsy
Accurate diagnosis is crucial in managing accessory nerve palsy. Healthcare professionals employ different methods to assess an individual’s condition and determine the most appropriate treatment options.
Clinical Examination and History
During a clinical examination, the healthcare provider will assess the range of motion in the head, neck, and shoulders. They will also evaluate muscle strength, coordination, and any associated symptoms. A detailed medical history, including information about potential causes and prior treatments, is essential in guiding the diagnosis.
When examining the range of motion in the head, the healthcare provider will ask the patient to perform various movements, such as turning the head from side to side and tilting it up and down. This helps to assess the function of the accessory nerve, which controls the movement of the trapezius and sternocleidomastoid muscles.
In addition to evaluating muscle strength, the healthcare provider may also perform specific tests to assess the function of the accessory nerve. For example, they may ask the patient to shrug their shoulders against resistance or turn their head against resistance. These tests help to determine if there is weakness or paralysis of the affected muscles.
Diagnostic Tests and Procedures
Diagnostic tests and procedures may be necessary to confirm the diagnosis of accessory nerve palsy and rule out other possible conditions. These may include imaging studies such as magnetic resonance imaging (MRI), electromyography (EMG) to assess nerve and muscle activity, and nerve conduction studies to evaluate the integrity of the nerve.
Magnetic resonance imaging (MRI) is a non-invasive imaging technique that uses a strong magnetic field and radio waves to create detailed images of the structures inside the body. It can help identify any structural abnormalities or lesions that may be affecting the accessory nerve.
Electromyography (EMG) involves the insertion of small needles into the muscles to record the electrical activity produced by the muscles and the nerves that control them. This test can help determine if there is any damage or dysfunction in the accessory nerve or the muscles it innervates.
Nerve conduction studies involve the application of small electrical impulses to the nerve and recording the response. This test can help assess the speed and strength of the nerve signals, which can provide information about the integrity of the accessory nerve.
In some cases, additional tests may be necessary to rule out other conditions that can cause similar symptoms to accessory nerve palsy. These may include blood tests, such as thyroid function tests, to check for any underlying metabolic or hormonal abnormalities.
Overall, a combination of clinical examination, medical history, and diagnostic tests is essential in accurately diagnosing accessory nerve palsy. This comprehensive approach helps healthcare professionals develop an appropriate treatment plan tailored to the individual’s specific needs.
Treatment Options for Accessory Nerve Palsy
Accessory nerve palsy is a condition that can cause significant discomfort and limitations in daily activities. Fortunately, there are various treatment options available to individuals with this condition. The choice of treatment depends on several factors, including the underlying cause, severity of symptoms, and individual circumstances.
Non-Surgical Treatments
In less severe cases of accessory nerve palsy, non-surgical treatments may be employed. These treatments aim to alleviate symptoms and improve overall function without the need for invasive procedures.
One common non-surgical treatment option is physical therapy. This approach involves targeted exercises and techniques that aim to strengthen the affected muscles and improve range of motion. Physical therapists work closely with individuals to develop personalized treatment plans that address their specific needs and goals.
In addition to physical therapy, pain management techniques may also be recommended. This can include the use of medication to alleviate pain and reduce inflammation. Therapeutic modalities, such as heat or cold therapy, electrical stimulation, or ultrasound, may also be utilized to provide relief and promote healing.
It is important for individuals with accessory nerve palsy to seek guidance from a healthcare professional to determine the most suitable non-surgical treatment approach. A thorough evaluation of the individual’s condition and symptoms will help determine the most effective course of action.
Surgical Treatments
In more severe cases of accessory nerve palsy or instances where conservative treatment options have not been effective, surgical intervention may be considered. Surgical procedures can offer a more direct approach to addressing the underlying cause of the condition and restoring normal nerve function.
One common surgical procedure for accessory nerve palsy is nerve repair. This involves reconnecting the damaged or severed nerve fibers to restore their function. The success of this procedure depends on several factors, including the extent of nerve damage and the individual’s overall health.
In cases where nerve repair is not possible, nerve reconstruction may be considered. This procedure involves using a nerve graft or transferring a healthy nerve from another part of the body to replace the damaged section. Nerve reconstruction can be a complex procedure that requires the expertise of a skilled surgeon.
Individuals considering surgical treatment for accessory nerve palsy should consult with a medical professional who specializes in this field. They will guide individuals through the decision-making process, discussing the potential risks, benefits, and expected outcomes of the procedure.
In conclusion, treatment options for accessory nerve palsy range from non-surgical approaches, such as physical therapy and pain management techniques, to surgical interventions like nerve repair or reconstruction. The choice of treatment depends on various factors and should be made in consultation with a healthcare professional. With proper treatment and care, individuals with accessory nerve palsy can experience improved function and a better quality of life.
Living with Accessory Nerve Palsy
Living with accessory nerve palsy can pose challenges, but there are strategies and support systems that can help individuals manage their condition effectively.
Coping Mechanisms and Strategies
Developing coping mechanisms and strategies can help individuals navigate the physical and emotional aspects of living with accessory nerve palsy. These may include adopting adaptive techniques for daily activities, seeking support from healthcare professionals, and connecting with support groups to share experiences and information.
Rehabilitation and Physical Therapy
Rehabilitation and physical therapy play a crucial role in the recovery process for individuals with accessory nerve palsy. These therapies aim to improve muscle strength, range of motion, and overall function. Working closely with a trained therapist can help individuals regain independence and enhance their quality of life.
Prevention and Prognosis
While it may not always be possible to prevent accessory nerve palsy, there are measures individuals can take to minimize their risk and improve their prognosis.
Preventive Measures
Engaging in activities with a lower risk of neck or shoulder injuries, practicing safe driving habits, and utilizing proper protective gear during sports can help reduce the likelihood of physical trauma that may lead to palsy. Additionally, managing underlying medical conditions and seeking prompt medical attention for infections or tumors can contribute to preventing accessory nerve palsy.
Prognosis and Long-Term Outlook
The prognosis for individuals with accessory nerve palsy varies depending on the cause, severity of symptoms, and individual response to treatment. While some individuals may experience full recovery, others may have residual symptoms. Working closely with healthcare professionals and following recommended treatments and therapies can optimize the long-term outlook for individuals with accessory nerve palsy.
If you suspect you may be experiencing symptoms of accessory nerve palsy, it is important to consult with a healthcare professional. They can provide an accurate diagnosis, guide the appropriate treatment options, and support you throughout your journey towards recovery and improved quality of life.


