how to assess the spinal accessory nerve
The spinal accessory nerve plays a crucial role in neck and shoulder movement, and assessing its function is essential for diagnosing and managing related disorders and conditions. In this article, we will discuss the anatomy and function of the spinal accessory nerve, the importance of assessing it, the clinical examination process, interpretation of examination results, advanced diagnostic procedures, treatment options, and rehabilitation approaches.
Understanding the Spinal Accessory Nerve
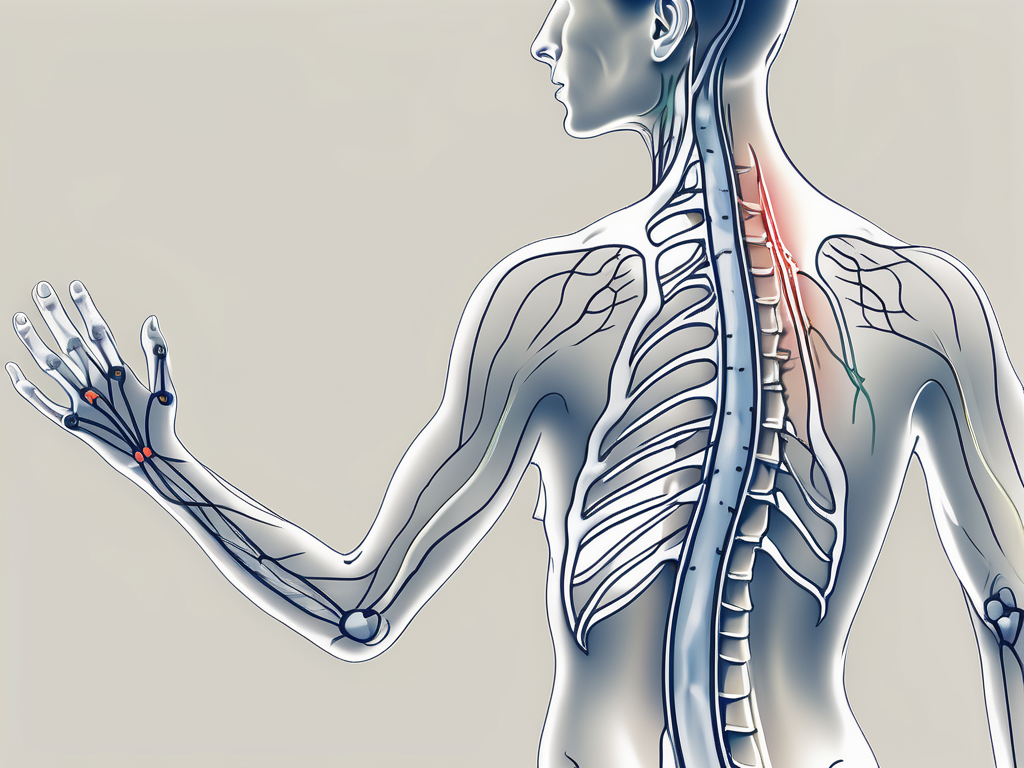
The spinal accessory nerve, also known as cranial nerve XI, is a motor nerve that originates from the upper spinal cord in the neck. It consists of two components: the cranial component and the spinal component.
The cranial component arises from the lower part of the brainstem and travels through the skull to join with the spinal component. This intricate pathway allows for the integration of motor signals from the brain to the neck and shoulder region.
The spinal component emerges from the skull and joins the cranial component in the neck, forming the main trunk of the spinal accessory nerve. This union of the two components ensures the efficient transmission of motor signals to the target muscles.
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve is a fascinating structure with a complex anatomy. It courses through various anatomical landmarks, providing a vital connection between the brain and the muscles it innervates.
As the cranial component of the spinal accessory nerve travels through the skull, it navigates through intricate bony canals and passes close to important structures such as the jugular foramen. This close proximity to other cranial nerves and blood vessels highlights the intricate nature of the nerve’s pathway.
Upon reaching the neck, the spinal component of the spinal accessory nerve joins the cranial component, forming a robust trunk. This trunk then continues its journey, branching out to innervate the sternocleidomastoid muscle and the trapezius muscle.
The sternocleidomastoid muscle, located in the front of the neck, plays a crucial role in head movement. It allows for rotation and tilting of the head, enabling us to look in different directions and maintain proper posture.
The trapezius muscle, on the other hand, is a large muscle that spans the upper back and neck region. It controls the movement of the shoulder blades, allowing for actions such as shrugging, pulling the shoulders back, and rotating the scapulae.
Function of the Spinal Accessory Nerve
The spinal accessory nerve plays a vital role in the coordination of movements in the neck and shoulder region. Its innervation of the sternocleidomastoid and trapezius muscles allows for precise control and coordination of these important structures.
When the spinal accessory nerve is functioning optimally, it ensures smooth and effortless movements of the head and shoulder blades. This coordination is essential for various activities, including looking around, maintaining balance, and performing tasks that involve the upper body.
However, damage or dysfunction of the spinal accessory nerve can lead to a range of symptoms. Weakness, muscle wasting, pain, and limited movement in the neck and shoulder region may occur as a result of compromised nerve function.
Understanding the intricacies of the spinal accessory nerve is crucial in diagnosing and managing conditions that affect its function. By comprehending its anatomy and function, healthcare professionals can provide targeted interventions to help patients regain optimal motor control and improve their quality of life.
Importance of Assessing the Spinal Accessory Nerve
Role in Neck and Shoulder Movement
The spinal accessory nerve, also known as cranial nerve XI, is a crucial component in coordinating the movement of the neck and shoulder muscles. It works in conjunction with other nerves and muscles to ensure smooth and coordinated motion in these areas. Without the proper functioning of the spinal accessory nerve, individuals may experience difficulties in performing everyday tasks that involve neck and shoulder movements.
When assessing the spinal accessory nerve, healthcare professionals evaluate its function by observing the range of motion in the neck and shoulder joints. They may also perform specific tests to determine the strength and coordination of the muscles controlled by this nerve. This assessment helps in diagnosing the cause of any movement difficulties or abnormalities that the patient may be experiencing.
If you find yourself experiencing weakness, pain, or restricted movement in your neck or shoulder area, it is essential to consult a healthcare professional who can perform a thorough assessment. This assessment will help determine the underlying cause of your symptoms and guide the appropriate treatment plan.
Implications of Spinal Accessory Nerve Damage
Damage to the spinal accessory nerve can occur due to various causes, including trauma, surgical procedures, or underlying medical conditions. Understanding the implications of such damage is necessary to develop an appropriate treatment plan and improve the quality of life for affected individuals.
One common condition associated with spinal accessory nerve damage is accessory nerve palsy. This condition occurs when the nerve is injured or compressed, leading to weakness or paralysis of the muscles it controls. This can result in difficulties with raising the arm, turning the head, or performing other movements involving the neck and shoulder.
Neck and shoulder injuries, such as whiplash or fractures, can also damage the spinal accessory nerve. In these cases, the nerve may be stretched, torn, or compressed, leading to a range of symptoms including pain, weakness, and limited mobility.
Tumors in the neck or shoulder region can also affect the spinal accessory nerve. As the tumor grows, it may put pressure on the nerve, causing pain, weakness, or other neurological symptoms. Prompt assessment and management of such tumors are crucial to prevent further damage and ensure the best possible outcome for the patient.
In addition to trauma and tumors, nerve entrapment syndromes can also cause damage to the spinal accessory nerve. These syndromes occur when the nerve gets trapped or compressed by surrounding structures, such as muscles or bones. This can lead to symptoms such as pain, numbness, tingling, and muscle weakness.
Each condition associated with spinal accessory nerve damage requires individualized assessment and management. Treatment options may include physical therapy, medication, nerve blocks, or, in severe cases, surgical intervention. The goal of treatment is to restore function, alleviate pain, and improve the overall quality of life for individuals affected by spinal accessory nerve damage.
Clinical Examination of the Spinal Accessory Nerve
Preparing for the Examination
Prior to the clinical examination, a thorough medical history will be obtained to understand your symptoms, previous injuries, and relevant medical conditions. This will help the examiner gain a comprehensive understanding of your health background and any potential factors that may contribute to spinal accessory nerve dysfunction.
Physical examinations may be conducted by a neurologist, orthopedic specialist, or physiotherapist. These healthcare professionals are trained to assess and diagnose conditions related to the nervous system, musculoskeletal system, and physical function.
It is important to inform the examiner about any recent surgeries, medications, or allergies to ensure a safe and effective examination. This information will help the examiner tailor the examination techniques and make any necessary adjustments to accommodate your specific needs.
Techniques for Physical Examination
The physical examination involves a systematic evaluation of the muscles and nerves associated with the spinal accessory nerve. The examiner will utilize various techniques to assess the function and integrity of this nerve, as well as the surrounding structures.
The examiner will begin by assessing the strength, range of motion, and coordination of your neck and shoulder muscles. This may involve resistance tests, where the examiner applies gentle pressure against specific muscle groups to evaluate their strength and response.
Additionally, muscle palpation will be performed to identify any areas of tenderness or abnormalities. By applying pressure and feeling the muscles, the examiner can gather valuable information about the condition of the spinal accessory nerve and its associated structures.
Range of motion measurements will also be conducted to assess the flexibility and mobility of your neck and shoulders. This may involve asking you to perform various movements, such as rotating your head or lifting your arms, while the examiner observes and records the range of motion achieved.
In some cases, special tests may be performed to target specific muscle groups and assess their function. These tests are designed to elicit specific responses and provide further insight into the condition of the spinal accessory nerve. The examiner will carefully guide you through these tests, ensuring your safety and comfort throughout the process.
During the examination, the examiner will also be on the lookout for any signs of muscle wasting, asymmetry, or abnormal movements. These observations can provide important clues about the nature and extent of the spinal accessory nerve dysfunction.
It is important to follow the examiner’s instructions carefully and communicate any discomfort or pain during the examination. Your feedback is crucial in ensuring a thorough and accurate assessment of your condition. By providing open and honest communication, you can help the examiner make informed decisions and recommendations based on your individual needs.
Ultimately, the results of the clinical examination will help determine the extent and nature of the spinal accessory nerve dysfunction. This information will guide the development of an appropriate treatment plan tailored to your specific condition, with the goal of improving your overall function and quality of life.
Interpreting Examination Results
After the examination, the healthcare professional will interpret the findings and compare them to the expected normal function of the spinal accessory nerve. Any deviations from the norm may indicate nerve damage or dysfunction.
Normal findings typically include symmetrical strength, full range of motion, and coordinated movements of the neck and shoulder muscles. This means that both sides of the body should exhibit similar levels of strength and flexibility, and the movements should be smooth and coordinated.
Abnormal findings may include muscle weakness, restricted movement, or other signs of nerve involvement. Muscle weakness can manifest as difficulty in performing certain movements or tasks that require the use of the neck and shoulder muscles. Restricted movement may be observed when the range of motion of the neck and shoulder is limited, causing discomfort or pain.
The examination results are essential for determining the underlying cause of the symptoms and guiding further diagnostic procedures or treatment options. By identifying any abnormalities in the spinal accessory nerve, healthcare professionals can develop an appropriate plan of action to address the issue.
Potential Disorders and Conditions
Based on the examination results, the healthcare professional may identify potential disorders or conditions related to spinal accessory nerve dysfunction. These can range from mild muscle strains to more severe nerve injuries or systemic diseases.
Mild muscle strains can occur due to overuse or improper use of the neck and shoulder muscles. This can result in temporary discomfort and limited range of motion. On the other hand, severe nerve injuries can lead to long-term or permanent damage to the spinal accessory nerve, causing significant weakness and functional impairment.
In some cases, spinal accessory nerve dysfunction may be a symptom of an underlying systemic disease. Conditions such as autoimmune disorders, infections, or tumors can affect the nerve’s function and lead to various symptoms.
Further diagnostic procedures such as electromyography and nerve conduction studies or imaging techniques like MRI or ultrasound may be recommended to confirm the diagnosis and assess the extent of the nerve damage. These tests can provide more detailed information about the nerve’s function and help healthcare professionals determine the most appropriate course of treatment.
It is important to consult with a healthcare professional for an accurate diagnosis and appropriate management options. They will be able to provide personalized recommendations based on the individual’s specific condition and needs.
Advanced Diagnostic Procedures
When it comes to diagnosing nerve and muscle function, advanced diagnostic procedures play a crucial role in providing detailed information. Two such procedures are electromyography (EMG) and nerve conduction studies (NCS).
Electromyography and Nerve Conduction Studies
EMG involves the insertion of tiny needles into the muscles to assess the electrical activity. By measuring the electrical signals produced by the muscles, EMG can help identify any abnormalities or dysfunctions. This procedure is particularly useful in diagnosing conditions such as muscle disorders, nerve compression, and peripheral neuropathy.
On the other hand, NCS evaluates the speed and efficiency of nerve signals as they travel through the affected area. By stimulating the nerves with small electrical impulses and measuring the response, NCS can determine the integrity of the nerves and identify any areas of nerve damage or dysfunction. This procedure is commonly used to diagnose conditions such as carpal tunnel syndrome, peripheral neuropathy, and nerve injuries.
Together, EMG and NCS provide a comprehensive assessment of nerve and muscle function, helping healthcare professionals pinpoint the specific location and severity of nerve damage.
Imaging Techniques for the Spinal Accessory Nerve
When it comes to assessing the spinal accessory nerve and its surrounding structures, imaging techniques play a vital role in providing detailed visuals.
Magnetic resonance imaging (MRI) is a non-invasive imaging technique that uses a powerful magnetic field and radio waves to create high-resolution images of the body’s internal structures. By capturing detailed cross-sectional images, MRI can help visualize any structural abnormalities or abnormalities that may be contributing to the nerve dysfunction. This imaging method is particularly useful in identifying tumors, nerve compression, and other structural issues affecting the spinal accessory nerve.
Ultrasound, on the other hand, is a real-time imaging technique that uses high-frequency sound waves to generate images of the body’s internal structures. By transmitting sound waves into the body and capturing the echoes, ultrasound can provide dynamic images of the spinal accessory nerve and surrounding tissues. This imaging method is particularly useful in assessing the nerve in real-time, allowing healthcare professionals to observe its function and detect any abnormalities or dysfunctions.
By utilizing these advanced imaging techniques, healthcare professionals can gain valuable insights into the condition of the spinal accessory nerve, aiding in the diagnosis and treatment of various nerve-related disorders.
Treatment Options for Spinal Accessory Nerve Damage
Conservative Management Strategies
In less severe cases, conservative management strategies may be recommended to alleviate symptoms and promote nerve recovery. This can include rest, physical therapy, pain management techniques, and lifestyle modifications.
Physical therapy approaches such as strengthening exercises, stretching, and manual therapy can help improve muscle function, reduce pain, and restore range of motion.
It is important to work closely with a healthcare professional to develop an individualized treatment plan that addresses your specific needs and goals.
Surgical Interventions
In more severe cases of spinal accessory nerve damage, surgical interventions may be necessary. The specific surgical procedure will depend on the underlying cause and extent of the nerve injury.
Examples of surgical interventions include nerve repair or grafting, decompression of nerve entrapment sites, or tumor removal. These procedures aim to alleviate nerve compression or repair damaged nerve structures.
It is crucial to consult with a specialist and discuss the potential risks, benefits, and expected outcomes of any surgical intervention.
Rehabilitation and Recovery
Physical Therapy Approaches
Physical therapy plays a vital role in the rehabilitation and recovery process of spinal accessory nerve damage. A skilled physiotherapist can design a personalized rehabilitation program based on your specific needs and goals.
The program may include exercises to improve strength, range of motion, and coordination, as well as techniques to manage pain and optimize function.
Adherence to the recommended exercises and following the guidance of the physiotherapist are critical for the success of the rehabilitation process.
Long-term Prognosis and Management
The long-term prognosis and management of spinal accessory nerve damage depend on various factors such as the underlying cause, severity of the nerve injury, and individual characteristics.
In some cases, complete recovery may be achieved with appropriate treatment and rehabilitation. However, in other cases, residual symptoms or functional limitations may persist.
Regular follow-up appointments with a healthcare professional are necessary for monitoring progress, adjusting treatment strategies, and managing any potential complications.
Conclusion
The assessment of the spinal accessory nerve is essential in diagnosing and managing related conditions. Understanding its anatomy, function, and clinical examination process provides valuable insights into the underlying cause of symptoms and guides appropriate treatment and rehabilitation approaches.
If you experience any symptoms or difficulties related to neck or shoulder movement, it is crucial to consult with a healthcare professional for a comprehensive evaluation and personalized management plan.


