what happens when there is damage to accessory nerve

The accessory nerve, also known as the cranial nerve XI, plays a crucial role in the coordination of certain movements and functions in the human body. When this nerve sustains damage, it can lead to various complications and impairments. Understanding the anatomy, function, causes, symptoms, diagnosis, treatment options, prognosis, and prevention of accessory nerve damage is essential for individuals who may be at risk or currently experiencing such issues. In this article, we will delve into each of these aspects to provide you with a comprehensive overview.
Understanding the Accessory Nerve
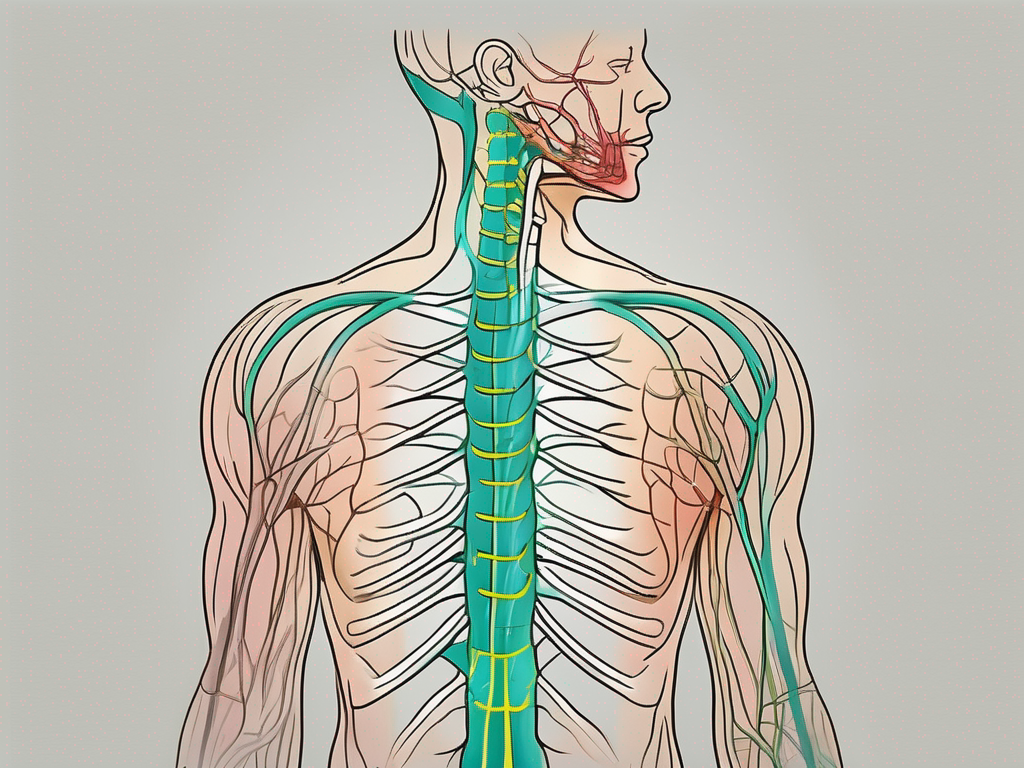
The accessory nerve, also known as the eleventh cranial nerve (CN XI), is a motor nerve that plays a crucial role in controlling specific muscles in the neck and shoulders. To fully comprehend the significance of this nerve, it is essential to explore its anatomy and function in detail.
Anatomy of the Accessory Nerve
The accessory nerve consists of two distinct parts: the cranial portion and the spinal portion.
The cranial portion of the accessory nerve originates from the nucleus ambiguus, a collection of motor neurons located in the medulla oblongata. These motor neurons serve as the starting point for the cranial fibers of the nerve.
The spinal portion of the accessory nerve, on the other hand, arises from the upper segments of the spinal cord. It emerges from the spinal cord’s roots, specifically from the region between the first and fifth cervical vertebrae. This spinal component of the accessory nerve is responsible for a significant portion of its motor function.
Once the cranial and spinal portions of the accessory nerve have originated, they converge and form a single nerve trunk. This nerve trunk then descends through the neck, passing through various structures and regions before reaching its target muscles.
Function of the Accessory Nerve
The primary function of the accessory nerve is to control the movement of specific muscles involved in the rotation and shrugging of the shoulders, as well as the turning of the head. These muscles include the sternocleidomastoid and trapezius muscles.
The sternocleidomastoid muscle, located on each side of the neck, plays a crucial role in tilting and rotating the head. When the accessory nerve sends signals to this muscle, it allows for controlled and coordinated movements of the head in various directions.
The trapezius muscle, which spans across the upper back and neck, is responsible for the elevation, depression, retraction, and rotation of the scapulae (shoulder blades). The accessory nerve innervates this muscle, enabling precise movements of the shoulders and upper back.
It is important to note that the accessory nerve does not work in isolation. It collaborates with other cranial nerves, such as the facial nerve (CN VII) and the glossopharyngeal nerve (CN IX), to ensure proper coordination and execution of movements involving the head, neck, and shoulders.
In conclusion, the accessory nerve is a vital component of the nervous system, responsible for controlling specific muscles in the neck and shoulders. Its anatomy, consisting of cranial and spinal portions, allows for the precise coordination of movements involved in head rotation, shoulder shrugging, and the turning of the head. Understanding the intricate details of this nerve enhances our knowledge of the human body’s complexity and the remarkable interplay between various anatomical structures.
Causes of Accessory Nerve Damage
The accessory nerve, also known as cranial nerve XI, plays a crucial role in controlling the movement of certain muscles in the neck and shoulders. Damage to this nerve can result in various symptoms, including weakness, pain, and limited range of motion. While the causes of accessory nerve damage can vary, they often involve trauma, surgical complications, or certain neurological disorders.
Trauma and Injury
One of the primary causes of accessory nerve damage is trauma or injury to the neck or shoulders. This can occur due to car accidents, falls, sports injuries, or any other event that exerts excessive force on the nerve, leading to stretching, compression, or laceration.
For example, in the case of a car accident, the sudden impact can cause the head and neck to jerk forcefully, potentially damaging the accessory nerve. Similarly, a fall from a significant height can result in direct trauma to the neck or shoulders, affecting the nerve’s integrity.
It is important to note that the severity of the trauma or injury can influence the extent of the nerve damage. In some cases, the nerve may only experience temporary dysfunction, while in others, it may sustain permanent damage.
Surgical Complications
During surgical procedures involving the neck or cervical spine, there is a risk of unintentional damage to the accessory nerve. This can happen during lymph node removal, tumor resection, or other surgical interventions in the region.
Surgeons take great care to avoid injuring the accessory nerve during these procedures. However, due to the complex anatomy and proximity of the nerve to other structures, there is always a possibility of accidental damage. In some cases, the nerve may be directly cut or compressed by surgical instruments or affected by post-operative swelling and inflammation.
It is worth mentioning that the risk of accessory nerve damage during surgery is relatively low, and most surgical interventions are successful without any complications. However, patients should be aware of the potential risks and discuss them with their healthcare providers before undergoing any procedures.
Neurological Disorders
In rare cases, certain neurological disorders, such as motor neuron diseases or autoimmune conditions, can affect the accessory nerve. These disorders can lead to degeneration or inflammation of the nerve, compromising its function.
Motor neuron diseases, including amyotrophic lateral sclerosis (ALS), can cause progressive damage to the nerves that control voluntary muscle movements, including the accessory nerve. As the disease progresses, the nerve may become less responsive, leading to muscle weakness and atrophy.
Autoimmune conditions, such as Guillain-Barré syndrome, can also target the peripheral nerves, including the accessory nerve. In these cases, the immune system mistakenly attacks the nerve fibers, resulting in inflammation and disruption of nerve signals.
It is important to note that neurological disorders affecting the accessory nerve are relatively uncommon. However, individuals with a known history of such conditions should be aware of the potential impact on their accessory nerve function and seek appropriate medical care.
In conclusion, accessory nerve damage can occur due to trauma or injury, surgical complications, or certain neurological disorders. Understanding the causes and potential risks associated with accessory nerve damage is essential for early detection, proper management, and potential recovery.
Symptoms of Accessory Nerve Damage
Physical Manifestations
Damage to the accessory nerve can result in observable physical manifestations, such as weakness or atrophy of the muscles in the neck and shoulders. This can lead to difficulties in raising or turning the head, as well as limited shoulder movement on the affected side.
When the accessory nerve is damaged, it can have a significant impact on the overall functionality of the neck and shoulder muscles. The weakened or atrophied muscles may appear visibly smaller or less defined compared to the unaffected side. This can be a distressing sight for individuals who are experiencing this condition.
Furthermore, the weakness in the neck and shoulder muscles can make simple tasks like combing hair or putting on a shirt challenging. The affected individuals may struggle to lift their arms or rotate their head, leading to a loss of mobility and independence in daily activities.
Impact on Motor Skills
Individuals with accessory nerve damage may experience challenges in performing activities that involve shoulder and neck movements. This can include tasks like lifting objects, reaching overhead, or participating in sports or physical activities.
Engaging in physical activities that require the use of the accessory nerve can become frustrating and discouraging for those affected. Simple tasks like throwing a ball or swinging a golf club may be difficult or impossible, leading to a loss of enjoyment and participation in recreational activities.
Moreover, the impact on motor skills can extend beyond sports and physical activities. Simple tasks like driving a car or carrying groceries can become arduous and may require assistance from others. This loss of independence can have a profound effect on the individual’s quality of life and overall well-being.
Pain and Discomfort
In some cases, accessory nerve damage can cause pain and discomfort in the neck and shoulders. This can range from mild to severe, and may be accompanied by symptoms such as muscle spasms or stiffness.
The pain experienced by individuals with accessory nerve damage can be debilitating, affecting their ability to perform daily activities and impacting their overall quality of life. The constant discomfort can make it difficult to find a comfortable position while sitting, standing, or lying down, leading to disrupted sleep patterns and fatigue.
In addition to the pain, muscle spasms and stiffness can further exacerbate the discomfort. These involuntary contractions of the affected muscles can cause sudden and intense pain, making it challenging for individuals to engage in any physical movement without experiencing discomfort.
Diagnosis of Accessory Nerve Damage
When it comes to diagnosing accessory nerve damage, medical professionals employ a variety of techniques to ensure an accurate assessment. The process typically begins with a thorough evaluation of the individual’s medical history, delving into any previous injuries or surgeries that may have contributed to the current condition. This step is crucial in understanding the context and potential causes of the nerve damage.
Following the medical history review, a comprehensive physical examination is conducted. During this examination, the healthcare provider carefully assesses the patient’s muscle strength, range of motion, and other specific tests to determine the extent of nerve involvement. By observing the patient’s physical capabilities, the healthcare provider can gain valuable insights into the severity and location of the nerve damage.
Imaging Studies
In certain cases, additional diagnostic tools may be employed to aid in the diagnosis of accessory nerve damage. Imaging studies, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, are often requested to visualize the affected area in detail. These imaging techniques provide a comprehensive view of the nerves, muscles, and surrounding structures, enabling healthcare professionals to identify any abnormalities or potential causes of the symptoms.
MRI scans, which use powerful magnets and radio waves, produce detailed images of the body’s internal structures. This non-invasive procedure allows healthcare providers to examine the nerves and surrounding tissues with exceptional clarity. Similarly, CT scans utilize X-rays and computer technology to generate cross-sectional images, providing a different perspective on the affected area.
Laboratory Tests
In addition to imaging studies, healthcare providers may also order specific laboratory tests to assess nerve function and detect potential underlying conditions. These tests can provide valuable information about the overall health of the patient and help identify any contributing factors to the nerve damage.
One common laboratory test used in the diagnosis of nerve damage is electromyography (EMG). During an EMG, small electrodes are inserted into the muscles to measure their electrical activity. This test can help determine if the accessory nerve is functioning properly and identify any signs of nerve damage or dysfunction.
Furthermore, blood tests may be conducted to evaluate the levels of certain markers or substances that could indicate an underlying condition contributing to the nerve damage. These tests can provide valuable insights into the overall health of the patient and help guide the treatment plan.
Overall, the diagnosis of accessory nerve damage involves a comprehensive approach that combines medical history evaluation, physical examination, and the use of imaging studies and laboratory tests. By utilizing these various techniques, healthcare professionals can accurately assess the extent of the nerve damage and develop an appropriate treatment plan tailored to the individual’s needs.
Treatment Options for Accessory Nerve Damage
Accessory nerve damage can significantly impact a person’s quality of life, causing pain, weakness, and limited mobility. Fortunately, there are several treatment options available to manage this condition and promote recovery. In addition to the commonly prescribed medication and drug therapy, physical therapy and rehabilitation, as well as surgical interventions, can play a crucial role in restoring function and alleviating symptoms.
Medication and Drug Therapy
When it comes to accessory nerve damage, medication and drug therapy can be effective in managing pain, reducing inflammation, and addressing underlying conditions that may be contributing to the nerve damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often prescribed to alleviate pain and inflammation. Additionally, muscle relaxants may be recommended to relieve muscle spasms and promote relaxation. It is important to note that medication and drug therapy should always be prescribed and monitored by a healthcare professional to ensure safety and effectiveness.
Physical Therapy and Rehabilitation
Physical therapy is a cornerstone of treatment for individuals with accessory nerve damage. A customized program, tailored to the specific needs and abilities of the patient, can help improve muscle strength, range of motion, and coordination. Physical therapists employ various techniques and exercises to target specific muscle groups and promote functional recovery. These may include stretching exercises, resistance training, and balance exercises. In addition, modalities such as heat therapy, ultrasound, and electrical stimulation may be used to enhance the effectiveness of the treatment.
Physical therapy not only focuses on the affected area but also addresses any compensatory movements or imbalances that may have developed as a result of the nerve damage. By restoring proper movement patterns and alignment, physical therapy can help individuals regain their independence and improve their overall quality of life.
Surgical Interventions
In severe cases of accessory nerve damage where conservative treatments have not provided sufficient relief, surgical interventions may be considered. The decision to undergo surgery is typically based on the extent and location of the nerve injury, as well as the individual’s overall health and functional goals.
There are several surgical procedures that can be performed to repair or reconstruct the damaged accessory nerve. Nerve grafting, for example, involves taking a healthy nerve from another part of the body and using it to bridge the gap in the damaged nerve. This allows for the regrowth of nerve fibers and potential functional improvement.
In some cases, nerve transfer surgery may be recommended. This involves transferring a healthy nerve from a less critical muscle or nerve group to the affected area. By rerouting the nerve signals, this procedure can help restore muscle function and improve overall movement.
It is important to note that surgical interventions for accessory nerve damage are complex procedures that require a skilled and experienced surgeon. The decision to undergo surgery should be carefully considered and discussed with a healthcare professional to ensure the potential benefits outweigh the risks.
In conclusion, treatment options for accessory nerve damage are diverse and aim to alleviate pain, restore function, and improve overall quality of life. Medication and drug therapy, physical therapy and rehabilitation, as well as surgical interventions, can all play a crucial role in the management and recovery of individuals with this condition. It is important to consult with a healthcare professional to determine the most appropriate treatment plan based on individual needs and circumstances.
Prognosis and Recovery from Accessory Nerve Damage
Factors Influencing Recovery
The prognosis and recovery from accessory nerve damage vary depending on several factors. These include the severity and location of the injury, age, overall health, and adherence to recommended treatments and therapies. Each individual’s response to treatment may differ, and it is important to consult with a healthcare professional for personalized advice.
Coping and Management Strategies
Living with accessory nerve damage can present challenges, both physically and emotionally. It is important to develop coping mechanisms and management strategies to adapt to any limitations or changes in physical function. Seeking support from healthcare professionals and engaging in activities that promote overall well-being can contribute to a positive outlook and improved quality of life.
Preventing Accessory Nerve Damage
Safety Measures and Precautions
Preventing accessory nerve damage primarily involves practicing safety measures and precautions in activities that carry a risk of neck or shoulder injury. This can include wearing appropriate protective gear during sports, maintaining proper posture, and avoiding excessive strain on the neck or shoulders in daily activities.
Regular Check-ups and Early Detection
Regular check-ups with a healthcare professional can help detect any potential issues or underlying conditions that may contribute to accessory nerve damage. Early detection and intervention can facilitate prompt treatment and minimize the risk of complications.
In conclusion, damage to the accessory nerve can lead to various complications and impairments, affecting the movement and function of certain neck and shoulder muscles. Understanding the anatomy, causes, symptoms, diagnosis, treatment options, prognosis, and prevention of accessory nerve damage is crucial for individuals at risk or currently experiencing such challenges. Consultation with a medical professional is essential to obtain an accurate diagnosis and develop an appropriate treatment plan tailored to individual needs. By staying informed and proactive, individuals can improve their chances of managing and recovering from accessory nerve damage effectively.