what happens to resting position of scapula if the motor accessory nerve is damaged
The human body is a remarkable machine, with each part serving a specific purpose. One important component of our musculoskeletal system is the scapula, commonly known as the shoulder blade. The scapula plays a crucial role in the movement and stability of our shoulders, enabling us to perform a wide range of activities. But what happens to the resting position of the scapula if the motor accessory nerve is damaged?
Understanding the Role of the Motor Accessory Nerve
The motor accessory nerve, also known as the 11th cranial nerve, is responsible for controlling certain muscles involved in shoulder movement. This nerve originates from the spinal cord in the neck and passes through the skull to reach its destination. While the primary function of this nerve is to innervate the sternocleidomastoid and trapezius muscles, it also plays a crucial role in maintaining the resting position of the scapula.
The Motor Accessory Nerve and the Scapula
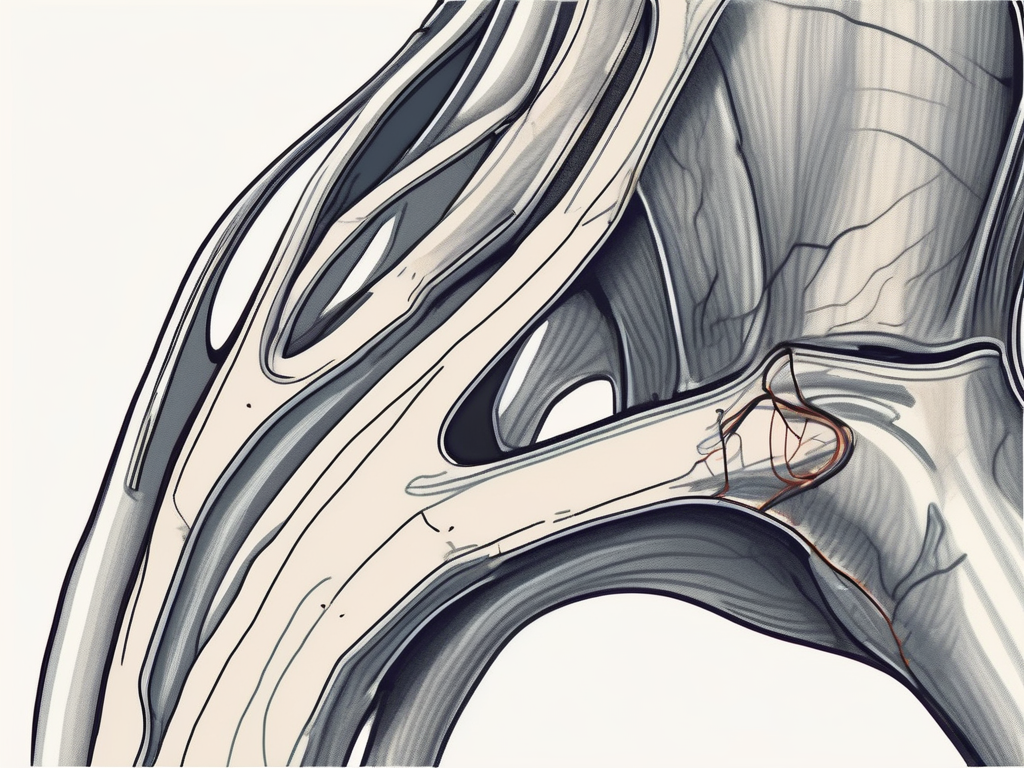
The scapula, commonly known as the shoulder blade, relies on a delicate balance of muscles for proper positioning during rest and movement. The trapezius muscle, innervated by the motor accessory nerve, is responsible for controlling the position of the scapula. This muscle spans across the back and neck, attaching to the spine and the clavicle. It plays a vital role in shoulder movement and stability.
When the motor accessory nerve is damaged, the trapezius muscle may experience weakness or paralysis, affecting the resting position of the scapula. This can lead to a variety of issues, including shoulder pain, limited range of motion, and difficulty performing daily activities that involve the use of the shoulder joint.
Furthermore, the motor accessory nerve also contributes to the innervation of the sternocleidomastoid muscle. This muscle is located in the front of the neck and is responsible for various movements, such as rotating and flexing the head. When the motor accessory nerve is compromised, it can result in weakness or paralysis of the sternocleidomastoid muscle, leading to difficulties in neck movements and potentially impacting overall posture.
The Impact of Nerve Damage on Muscle Function
Nerve damage can have significant implications for muscle function. In the case of motor accessory nerve damage, the affected muscles may not receive the necessary signals to contract or relax correctly. This can result in an imbalance of muscle forces, leading to abnormal scapular positioning.
Abnormal scapular positioning, also known as scapular dyskinesis, can have a cascading effect on the entire shoulder complex. It can lead to altered biomechanics, increased stress on surrounding structures, and a higher risk of shoulder injuries. Individuals with motor accessory nerve damage may experience difficulties in performing overhead activities, such as reaching or lifting objects, due to the compromised stability and coordination of the shoulder joint.
Rehabilitation and physical therapy play a crucial role in the management of motor accessory nerve damage. These interventions focus on strengthening the affected muscles, improving range of motion, and restoring proper scapular positioning. Additionally, techniques such as electrical stimulation and manual therapy may be utilized to facilitate nerve regeneration and enhance muscle function.
Understanding the role of the motor accessory nerve and its impact on muscle function is essential for healthcare professionals in diagnosing and treating shoulder-related conditions. By addressing nerve damage and promoting optimal muscle function, individuals can regain their shoulder mobility and improve their overall quality of life.
The Resting Position of the Scapula
The resting position of the scapula is an essential aspect of our body mechanics. When at rest, the scapula should be in a balanced and neutral position, allowing for efficient and pain-free movement. The scapula should sit flat against the ribcage, with the top edge, known as the superior angle, level with the second or third thoracic vertebra.
But what exactly does it mean for the scapula to be in a balanced and neutral position? Let’s dive deeper into the intricacies of scapular position and its importance in our overall body mechanics.
The Importance of Scapular Position in Body Mechanics
Proper scapular position is crucial for optimal shoulder joint function. A balanced resting position of the scapula ensures that the surrounding muscles work harmoniously, allowing for smooth movement and stability. It enables us to perform daily activities such as reaching, lifting, and pushing without undue stress on the surrounding structures.
Imagine trying to lift a heavy object with your scapula in an incorrect position. The muscles responsible for stabilizing the scapula and shoulder joint would be compromised, leading to inefficient movement and potential injury. By maintaining a balanced and neutral scapular position, we can enhance our overall body mechanics and reduce the risk of musculoskeletal issues.
How Nerve Damage Can Affect Scapular Position
While the resting position of the scapula is crucial for optimal body mechanics, certain conditions or injuries can disrupt this delicate balance. One such condition is nerve damage, specifically damage to the motor accessory nerve.
The motor accessory nerve plays a vital role in innervating the muscles responsible for scapular movement. When this nerve is damaged, the affected muscles may not function correctly, leading to an altered resting position of the scapula. One common manifestation of nerve damage is scapular winging.
Scapular winging refers to the abnormal protrusion of the scapula from the back, creating an unnatural appearance. This abnormal position can result in restricted shoulder movement, weakness, and pain. Imagine the challenges one would face in performing daily activities with a winged scapula. Simple tasks like combing your hair or reaching for a glass on a high shelf become arduous and painful.
It is crucial to address nerve damage and its impact on scapular position promptly. Physical therapy, targeted exercises, and other interventions can help restore proper scapular alignment and function, allowing individuals to regain pain-free movement and improve their overall quality of life.
In conclusion, the resting position of the scapula is not just a static anatomical detail but a critical factor in our body mechanics. By understanding the importance of scapular position and its potential disruption due to nerve damage, we can appreciate the significance of maintaining a balanced and neutral scapular position. So, let’s strive for optimal scapular alignment and empower ourselves with efficient and pain-free movement.
Symptoms of Motor Accessory Nerve Damage
Motor accessory nerve damage can manifest in various physical symptoms. Understanding these symptoms is crucial in identifying and addressing the issue promptly.
When the motor accessory nerve is damaged, it can lead to weakness or paralysis of the trapezius muscle. The trapezius muscle plays a vital role in shoulder movement and stability. When this muscle is affected, it can result in noticeable changes in scapular position and movement. Individuals may find it challenging to lift their arms or perform activities that require shoulder mobility.
In addition to weakness or paralysis of the trapezius muscle, motor accessory nerve damage can cause pain or discomfort in the neck and shoulder area. This pain may be sharp or dull and can radiate down the arm. The affected individual may also experience decreased muscle strength in the affected region, making it difficult to perform tasks that require strength and endurance.
Physical Symptoms and Their Causes
Weakness or paralysis of the trapezius muscle, which is innervated by the motor accessory nerve, is one of the primary symptoms of nerve damage. This can lead to noticeable changes in scapular position and movement. Additionally, individuals may experience difficulty lifting their arms, pain or discomfort in the neck and shoulder area, and decreased muscle strength in the affected region.
Motor accessory nerve damage can occur due to various causes. Trauma, such as a car accident or sports injury, can result in nerve damage. Inflammation or compression of the nerve can also lead to its impairment. Certain medical conditions, such as brachial plexus injuries or nerve entrapment syndromes, can affect the motor accessory nerve as well.
Long-Term Effects of Nerve Damage
If left untreated, long-term effects of motor accessory nerve damage can include chronic pain, muscle atrophy, and limited range of motion. Chronic pain can significantly impact an individual’s quality of life, making it challenging to perform daily activities and affecting sleep patterns. Muscle atrophy, the wasting away of muscle tissue, can occur when the nerve damage prevents proper muscle activation and use. This can lead to a decrease in muscle size and strength.
Furthermore, limited range of motion is a common long-term effect of motor accessory nerve damage. The affected individual may find it difficult to move their shoulder and perform certain movements, such as reaching overhead or behind their back. This limitation can hinder their ability to participate in sports, exercise, or even perform simple tasks like getting dressed.
It is essential to seek medical attention if you suspect motor accessory nerve damage. Early diagnosis and treatment can help prevent further complications and promote optimal recovery. Treatment options may include physical therapy, medication, or, in severe cases, surgery. A healthcare professional will evaluate the individual’s specific condition and develop a personalized treatment plan to address their symptoms and improve their overall function.
Diagnosis and Treatment of Motor Accessory Nerve Damage
Diagnosing and treating motor accessory nerve damage requires the expertise and guidance of a medical professional. Seeking timely medical evaluation can help determine the extent and cause of the nerve damage, enabling the implementation of appropriate treatment strategies.
Motor accessory nerve damage, also known as accessory nerve palsy, can occur due to various reasons such as trauma, surgical procedures, or underlying medical conditions. The motor accessory nerve, also called the 11th cranial nerve, controls the movement of certain muscles in the neck and shoulders. When this nerve is damaged, it can result in weakness or paralysis of these muscles, leading to difficulties in performing everyday activities.
Diagnostic Techniques for Nerve Damage
A thorough diagnostic assessment is necessary to evaluate motor accessory nerve damage accurately. This may involve a combination of medical history review, physical examination, electromyography (EMG), nerve conduction studies, and imaging tests.
During the medical history review, the healthcare professional will ask questions about the onset and progression of symptoms, any recent injuries or surgeries, and any underlying medical conditions. This information helps in understanding the potential causes of the nerve damage.
The physical examination involves assessing the strength, range of motion, and coordination of the affected muscles. The healthcare professional may also perform specific tests to evaluate the function of the motor accessory nerve, such as asking the patient to shrug their shoulders or turn their head against resistance.
Electromyography (EMG) and nerve conduction studies are specialized tests that can provide valuable information about the electrical activity and conduction of the nerves. These tests involve placing small electrodes on the skin or inserting fine needles into the muscles to measure the nerve signals and muscle responses.
In some cases, imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered to visualize the structures in the neck and shoulders and identify any abnormalities or compression of the motor accessory nerve.
Treatment Options and Rehabilitation for Nerve Damage
The treatment and rehabilitation of motor accessory nerve damage primarily depend on the cause, severity, and individual circumstances. The ultimate goal is to restore optimal muscle function and scapular positioning.
Treatment options may include physical therapy to strengthen the surrounding muscles and improve range of motion. Physical therapists can design personalized exercise programs to target the specific muscles affected by the nerve damage. These exercises may include stretching, resistance training, and functional movements to enhance muscle strength and coordination.
Medication for pain management may be prescribed to alleviate any discomfort or neuropathic pain associated with the nerve damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) or other pain medications may be recommended to reduce inflammation and relieve pain symptoms.
In severe cases of motor accessory nerve damage, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause and the extent of the nerve damage. Surgical options may include nerve repair, nerve grafting, or nerve transfer procedures to restore the function of the affected muscles.
Rehabilitation programs are designed to address specific symptoms and promote functional recovery under the guidance of healthcare professionals. These programs may include a combination of physical therapy, occupational therapy, and speech therapy, depending on the individual’s needs and goals.
It is important to note that the recovery from motor accessory nerve damage can vary from person to person. Some individuals may experience a complete recovery, while others may have residual weakness or limitations. Regular follow-up appointments with the healthcare professional are essential to monitor progress, make any necessary adjustments to the treatment plan, and provide ongoing support and guidance.
Prevention and Management of Nerve Damage
Prevention is always better than cure when it comes to nerve damage. While some causes, such as trauma, are unpredictable, adopting certain lifestyle changes can reduce the risk of nerve damage and promote overall well-being.
Nerve damage can occur due to various factors, including repetitive activities, poor posture, and excessive strain on the body. It is essential to take proactive measures to prevent such damage and maintain optimal nerve health.
Lifestyle Changes to Prevent Nerve Damage
Engaging in regular exercise that focuses on strengthening the muscles surrounding the shoulder can help prevent nerve damage. Exercises such as shoulder shrugs, lateral raises, and rows can improve muscle strength and stability, reducing the risk of nerve compression or injury.
In addition to exercise, maintaining good posture is crucial for preventing nerve damage. Slouching or hunching over can put unnecessary pressure on the nerves, leading to potential complications. By practicing proper posture, such as sitting up straight and aligning the spine, you can alleviate stress on the nerves and promote better overall spinal health.
Another important aspect of preventing nerve damage is taking breaks during repetitive activities. Whether you’re engaged in manual labor or spend long hours typing on a keyboard, giving your body regular breaks can help prevent overuse injuries and nerve compression. Stretching and moving around during breaks can also improve blood circulation and reduce the risk of nerve damage.
Avoiding excessive strain on the body is also crucial for preventing nerve damage. Whether it’s lifting heavy objects or engaging in strenuous activities, it’s important to listen to your body’s limits and avoid pushing yourself beyond what is safe. Using proper lifting techniques, such as bending at the knees and using your leg muscles, can also help distribute the weight evenly and reduce the strain on your nerves.
Coping Strategies for Living with Nerve Damage
Living with motor accessory nerve damage can be challenging, but adapting to the situation and implementing coping strategies can help improve quality of life. It’s important to remember that everyone’s experience with nerve damage is unique, and what works for one person may not work for another. However, there are some general strategies that can be beneficial:
Utilizing assistive devices can make daily tasks more manageable for individuals with nerve damage. Devices such as braces, splints, or ergonomic tools can provide support and reduce strain on the affected area. These devices can help individuals maintain their independence and continue their daily activities with less discomfort.
Finding ways to minimize stress on the affected area is also crucial for managing nerve damage. This can include modifying workstations or home environments to reduce repetitive motions or implementing ergonomic principles to create a more comfortable and supportive space.
Seeking support from healthcare professionals or support groups can provide valuable guidance and assistance. Physical therapists, occupational therapists, and other healthcare professionals can offer specialized exercises and techniques to manage nerve damage. Support groups can also provide a sense of community and understanding, allowing individuals to share their experiences and learn from others facing similar challenges.
In conclusion, when the motor accessory nerve is damaged, the resting position of the scapula can be compromised, leading to altered scapular positioning and potential functional limitations. Recognizing the symptoms, seeking appropriate medical evaluation, and exploring treatment options is vital for optimal recovery and the restoration of normal scapular mechanics. If you suspect motor accessory nerve damage or experience any concerning symptoms, it is crucial to consult with a healthcare professional for proper diagnosis and guidance. Remember, your health and well-being should always be a top priority.


