what is spinal accessory nerve palsy
Spinal accessory nerve palsy is a medical condition that affects the functionality of the spinal accessory nerve. This nerve, also known as cranial nerve XI, plays a crucial role in controlling certain movements of the head, neck, and shoulders. When the spinal accessory nerve is affected, it can lead to weakness or paralysis of the muscles responsible for these movements.
Understanding the Spinal Accessory Nerve
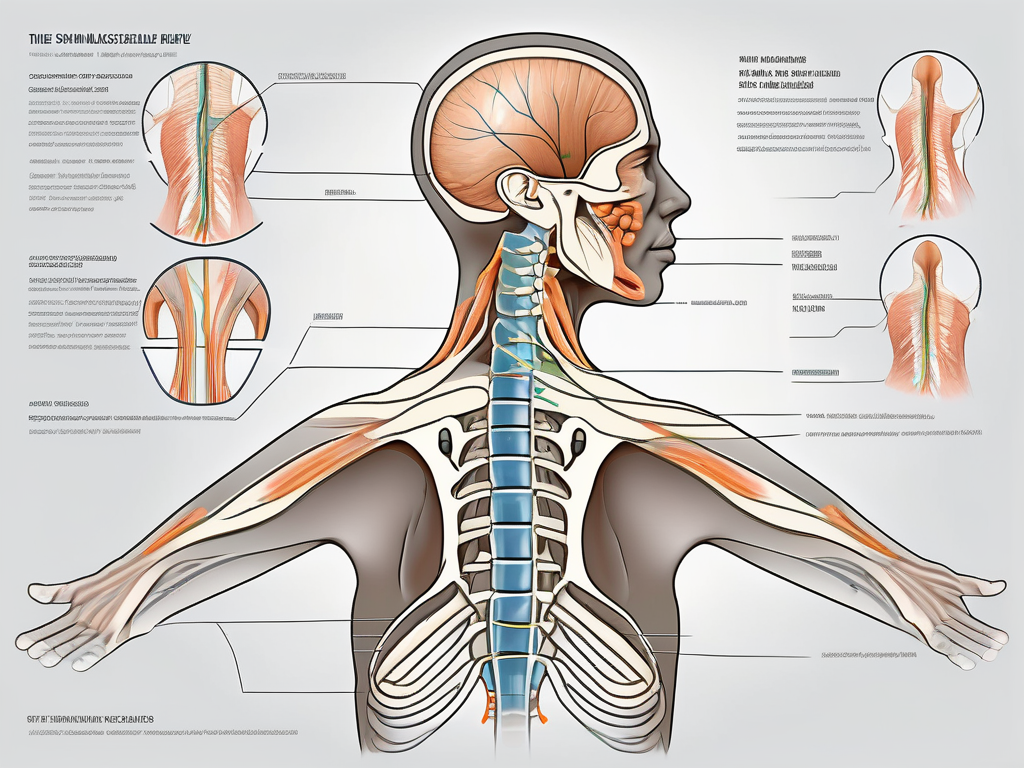
The spinal accessory nerve, also known as the eleventh cranial nerve, plays a crucial role in the motor function of the head, neck, and shoulders. Let’s delve deeper into the anatomy and function of this fascinating nerve.
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve originates from the brainstem, specifically from the upper part of the spinal cord. It consists of two distinct parts: the cranial part and the spinal part. The cranial part arises from the nucleus ambiguus in the medulla oblongata, while the spinal part emerges from the upper levels of the spinal cord.
These two parts of the spinal accessory nerve join together to form a single nerve trunk, which then travels through the neck. Along its course, it gives off branches that supply motor signals to various muscles involved in head, neck, and shoulder movements.
One of the remarkable features of the spinal accessory nerve is its unique pathway. Unlike other cranial nerves that directly exit the skull, the spinal accessory nerve exits the cranial cavity through the jugular foramen, a bony opening located at the base of the skull.
Function of the Spinal Accessory Nerve
The primary function of the spinal accessory nerve is to innervate two important muscles: the sternocleidomastoid muscle and the trapezius muscle.
The sternocleidomastoid muscle, named for its attachments to the sternum, clavicle, and mastoid process of the skull, plays a crucial role in head movements. It allows for rotation and flexion of the head, enabling us to turn our heads from side to side and tilt them forward and backward.
The trapezius muscle, named after its trapezoid shape, is a large muscle that spans the upper back and neck. It enables various movements of the shoulders and scapulae, including elevation, depression, retraction, and rotation. The trapezius muscle is essential for activities such as lifting the arms, maintaining proper posture, and stabilizing the shoulder girdle.
Both the sternocleidomastoid and trapezius muscles are vital for everyday activities. From the simple act of turning our heads to more complex movements like reaching overhead or carrying heavy objects, the spinal accessory nerve ensures the proper functioning of these muscles.
In addition to its role in motor function, the spinal accessory nerve also carries sensory fibers from the neck and shoulder region. These sensory fibers provide feedback to the central nervous system, allowing us to perceive sensations such as touch, pressure, and temperature in these areas.
Overall, the spinal accessory nerve is a remarkable structure that plays a crucial role in the intricate coordination of head, neck, and shoulder movements. Its intricate anatomy and diverse functions make it a fascinating subject of study for neuroscientists and healthcare professionals alike.
The Science Behind Spinal Accessory Nerve Palsy
The spinal accessory nerve, also known as cranial nerve XI, plays a crucial role in the motor function of the neck and shoulder muscles. When this nerve is damaged or disrupted, a condition known as spinal accessory nerve palsy can occur. In this expanded version, we will delve deeper into the causes and pathophysiology of this condition.
Causes of Spinal Accessory Nerve Palsy
Spinal accessory nerve palsy can occur due to various causes. One common cause is injury or trauma to the nerve during surgical procedures, particularly those involving the neck or shoulder area. This can happen when the nerve is accidentally cut, stretched, or compressed during the operation.
Another potential cause of spinal accessory nerve palsy is infections. Viral or bacterial infections affecting the nerve can lead to inflammation and damage. In some cases, the body’s immune response to the infection can mistakenly attack the nerve, resulting in palsy.
Furthermore, certain conditions can also contribute to the development of spinal accessory nerve palsy. Tumors in the neck or shoulder region can exert pressure on the nerve, interfering with its normal function. Nerve compression caused by herniated discs or other structural abnormalities can also lead to palsy.
Pathophysiology of Spinal Accessory Nerve Palsy
Understanding the pathophysiology of spinal accessory nerve palsy is essential in comprehending the functional impairments associated with this condition. When the spinal accessory nerve is damaged or disrupted, the transmission of motor signals from the brain to the affected muscles is compromised.
The spinal accessory nerve primarily innervates two important muscles: the sternocleidomastoid and the trapezius. The sternocleidomastoid muscle is responsible for rotating and tilting the head, while the trapezius muscle controls the movement of the shoulder blades and upper back.
When the spinal accessory nerve is impaired, the affected muscles may experience weakness or paralysis. This can result in difficulties in performing movements that require the involvement of the sternocleidomastoid and trapezius muscles. Simple actions like turning the head or lifting the arms may become challenging or even impossible.
The severity of spinal accessory nerve palsy can vary depending on the extent of nerve damage. In some cases, the palsy may be temporary, and the nerve can regenerate and regain its function over time. However, in more severe cases, the damage may be permanent, leading to long-term disability.
It is worth noting that the symptoms of spinal accessory nerve palsy can extend beyond motor impairments. Some individuals may also experience pain, numbness, or tingling sensations in the affected area. These sensory disturbances can further impact the quality of life for those living with this condition.
In conclusion, spinal accessory nerve palsy is a complex condition that can arise from various causes, including surgical injuries, infections, tumors, and nerve compression. Understanding the pathophysiology of this condition is crucial in developing effective treatment strategies and improving the overall management of patients with spinal accessory nerve palsy.
Identifying Spinal Accessory Nerve Palsy
Spinal accessory nerve palsy is a condition that can have a significant impact on a person’s daily life. It is important to be able to recognize the symptoms and signs of this condition in order to seek appropriate medical attention and treatment.
Symptoms and Signs
When someone is affected by spinal accessory nerve palsy, they may experience a range of symptoms and signs. One of the most common indications of this condition is weakness or paralysis of the affected muscles. This can lead to difficulties with head movement, making it challenging to turn the head from side to side or to look up and down. Additionally, shoulder elevation may be affected, making it difficult to raise the shoulders or perform certain movements involving the arms.
Another symptom that individuals with spinal accessory nerve palsy may experience is scapular stabilization issues. The scapula, or shoulder blade, plays a crucial role in shoulder movement and stability. When the spinal accessory nerve is affected, the muscles responsible for scapular stabilization may become weakened, leading to instability and potential discomfort.
In addition to these motor symptoms, patients with spinal accessory nerve palsy may also experience pain or discomfort in the affected areas. This can range from a dull ache to sharp, shooting pains that can significantly impact daily activities and quality of life.
Furthermore, in some cases, visible muscle atrophy or wasting may be observed. This occurs when the muscles affected by the spinal accessory nerve palsy begin to shrink and lose their normal bulk. Muscle atrophy can be a distressing symptom for patients, as it can further contribute to weakness and functional limitations.
Diagnostic Procedures
Diagnosing spinal accessory nerve palsy requires a thorough evaluation by a healthcare professional. The medical history of the patient is an essential component of the diagnostic process. The healthcare provider will inquire about any recent injuries or surgical procedures that may have contributed to the development of the condition.
In addition to the medical history, a physical examination will be conducted to assess the range of motion, strength, and stability of the affected areas. The healthcare provider will carefully observe the patient’s head movements, shoulder elevation, and scapular stabilization. Any visible muscle atrophy or wasting will also be noted.
To further evaluate the extent of nerve damage and to rule out other potential causes of the symptoms, additional diagnostic procedures may be recommended. These may include imaging tests such as magnetic resonance imaging (MRI) or electromyography (EMG). MRI can provide detailed images of the affected nerves and surrounding structures, allowing healthcare professionals to assess the extent of the damage. EMG, on the other hand, measures the electrical activity of the muscles, helping to determine the functionality of the affected nerves.
Overall, the diagnosis of spinal accessory nerve palsy requires a comprehensive approach, combining the patient’s medical history, physical examination, and potentially additional diagnostic procedures. This multi-faceted evaluation is crucial in order to accurately identify the condition and develop an appropriate treatment plan.
Treatment Options for Spinal Accessory Nerve Palsy
Non-Surgical Treatments
In many cases, non-surgical treatments are the first line of management for spinal accessory nerve palsy. These treatments focus on improving muscle strength and range of motion, as well as alleviating discomfort. Physical therapy exercises are often recommended to strengthen the affected muscles and improve overall function. These exercises may include specific movements and stretches that target the affected area, helping to restore muscle tone and flexibility.
Additionally, pain management techniques can be utilized to provide relief from discomfort. Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), may be prescribed to reduce inflammation and alleviate pain. Localized heat therapy, such as hot packs or warm compresses, can also be applied to the affected area to relax muscles and promote blood flow, which can help in reducing pain and promoting healing.
It is important to note that the choice of non-surgical treatments may vary depending on the individual’s specific needs and the severity of the nerve palsy. Consulting with a healthcare professional, such as a physical therapist or neurologist, is essential to determine the most appropriate non-surgical treatment approach.
Surgical Interventions
In severe cases or when non-surgical treatments do not provide satisfactory results, surgical interventions may be considered for spinal accessory nerve palsy. The specific surgical options can vary depending on the underlying cause of the nerve palsy and the individual’s unique circumstances.
One potential surgical option is nerve repair, which involves reconnecting the damaged or severed nerve ends. This procedure aims to restore nerve functionality and improve muscle strength. However, the success of nerve repair depends on various factors, such as the extent of the nerve damage and the individual’s overall health.
In cases where there is a significant gap between the damaged nerve ends, nerve grafts may be utilized. During a nerve graft procedure, a segment of nerve tissue is taken from another part of the body and used to bridge the gap between the damaged nerve ends. This allows for nerve regeneration and restoration of muscle function over time.
Another surgical technique that may be considered is nerve transfer. Nerve transfer involves taking a healthy nerve from a less critical muscle or area of the body and connecting it to the affected muscle. This allows for the transfer of nerve signals and can help restore muscle strength and function.
It is important to emphasize that the decision to undergo surgery for spinal accessory nerve palsy should be made in consultation with a specialist, such as a neurosurgeon or a plastic surgeon with expertise in nerve reconstruction. These specialists can assess the individual’s condition, discuss the potential risks and benefits of surgery, and determine the most suitable surgical approach.
In conclusion, the treatment options for spinal accessory nerve palsy range from non-surgical interventions, such as physical therapy exercises and pain management techniques, to surgical interventions, including nerve repair, nerve grafts, and nerve transfers. The choice of treatment depends on the severity of the nerve palsy, the underlying cause, and the individual’s specific needs. Consulting with a healthcare professional is crucial in determining the most appropriate treatment approach for optimal recovery and improved quality of life.
Living with Spinal Accessory Nerve Palsy
Spinal accessory nerve palsy is a condition that can significantly impact a person’s daily life. It affects the function of the spinal accessory nerve, which controls the movement of certain muscles in the neck and shoulder region. While living with this condition can be challenging, there are various strategies and therapies available to help individuals manage their symptoms and improve their overall quality of life.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation play a vital role in the management of spinal accessory nerve palsy. Under the guidance of a trained therapist, patients can learn specific exercises and techniques to enhance muscle function, improve coordination, and optimize overall quality of life. These exercises may include stretching, strengthening, and range-of-motion exercises that target the affected muscles.
In addition to exercises, physical therapists may also use other modalities such as heat or cold therapy, electrical stimulation, or ultrasound to help alleviate pain and promote healing. They may also provide education on proper body mechanics and ergonomics to prevent further injury and strain on the affected muscles.
Regular physical therapy sessions, supplemented by home exercises, can provide significant long-term benefits for individuals with spinal accessory nerve palsy. The exercises and techniques learned in therapy can help individuals regain strength, improve their range of motion, and enhance their overall functional abilities.
Coping Strategies and Support
Living with spinal accessory nerve palsy can be challenging both physically and emotionally. The impact of this condition on daily life can lead to feelings of frustration, isolation, and even depression. However, there are coping strategies and support systems available to help individuals navigate these challenges.
Engaging in support groups or seeking counseling can be beneficial for individuals coping with the impact of nerve palsy on their daily lives. Support groups provide a safe space for individuals to share their experiences, exchange tips and advice, and find emotional support from others who understand what they are going through. These groups can also provide valuable insights, encouragement, and a sense of belonging.
In addition to support groups, individual counseling can help individuals develop effective coping strategies and address any emotional challenges they may be facing. A counselor or therapist can provide guidance and support, helping individuals navigate the emotional impact of living with spinal accessory nerve palsy.
Furthermore, it is important for individuals with spinal accessory nerve palsy to have a strong support system in their personal lives. Family and friends can offer practical assistance, emotional support, and encouragement throughout the journey of managing this condition.
In conclusion, while living with spinal accessory nerve palsy can present challenges, there are various strategies and support systems available to help individuals manage their symptoms and improve their overall well-being. Through physical therapy, rehabilitation, coping strategies, and support from others, individuals can enhance their quality of life and find ways to adapt to the challenges posed by this condition.
Prevention and Risk Factors
Understanding the Risk Factors
While spinal accessory nerve palsy can occur as a result of various causes, certain risk factors may increase the likelihood of its development. These can include a history of previous neck or shoulder surgeries, prolonged pressure on the nerve during immobilization, or the presence of underlying conditions that affect nerve health.
Preventive Measures
While it may not always be possible to prevent spinal accessory nerve palsy, taking certain precautions can help reduce the risk. It is essential to communicate any relevant medical history or risk factors to healthcare professionals before undergoing surgeries or medical procedures. Maintaining good overall health, including regular exercise, a balanced diet, and appropriate body mechanics, can also contribute to nerve health.
In conclusion, spinal accessory nerve palsy is a condition that affects the functionality of the spinal accessory nerve, leading to weakness or paralysis of specific muscles involved in head, neck, and shoulder movements. Identifying and diagnosing the condition typically involves a comprehensive evaluation by a healthcare professional. Treatment options range from non-surgical approaches, such as physical therapy, to surgical interventions in severe cases. Living with spinal accessory nerve palsy can be managed with physical therapy and the support of counseling or support groups. While prevention may not always be possible, understanding the risk factors and adopting preventive measures can help minimize the chances of developing this condition. It is crucial to consult with a healthcare professional for an accurate diagnosis and tailored treatment plan that best suits individual needs.


