how does an accessory nerve injury affect the scapula
The scapula, also known as the shoulder blade, plays a crucial role in our ability to perform various movements of the upper extremity. Injury to the accessory nerve, also known as the 11th cranial nerve or the spinal accessory nerve, can have a significant impact on the functioning of the scapula. In this article, we will explore the anatomy and function of the accessory nerve, its link to the scapula, the symptoms and diagnosis of accessory nerve injury, the consequences of such an injury on scapula function, as well as the treatment and rehabilitation options available.
Understanding the Accessory Nerve and Its Function
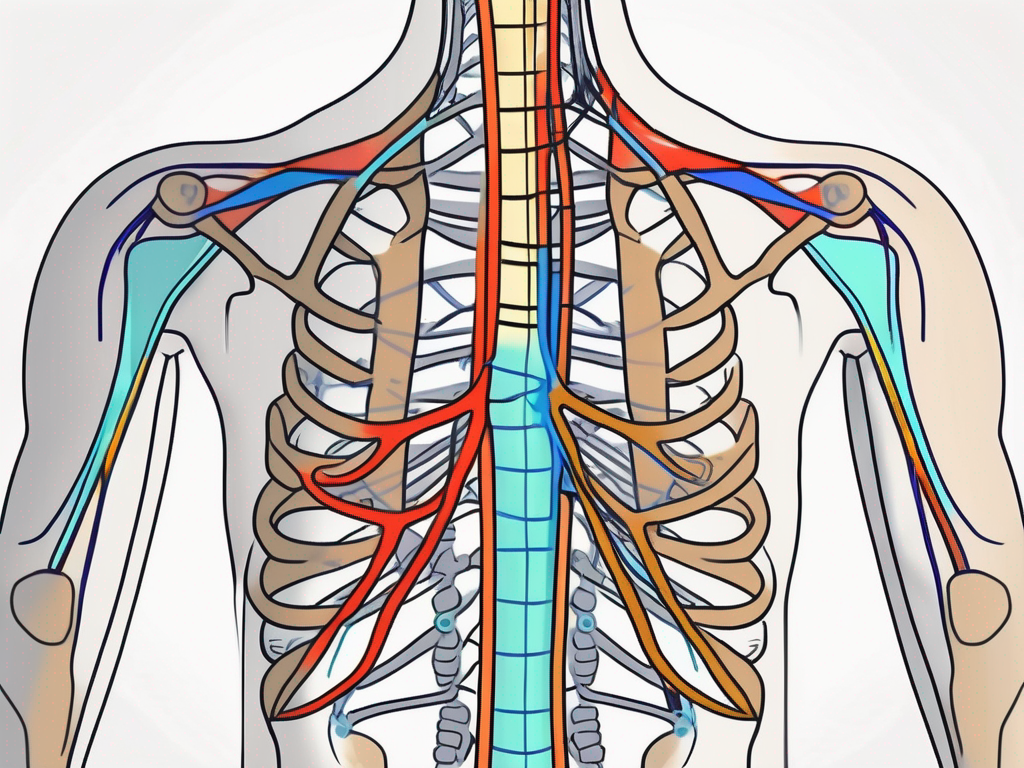
The accessory nerve is a motor nerve that originates from the spinal cord in the upper neck and plays a crucial role in innervating certain muscles involved in shoulder movement. It consists of two main components: the cranial component, which arises from the brainstem, and the spinal component, which arises from the upper spinal cord. The accessory nerve primarily innervates the trapezius and sternocleidomastoid muscles, which are responsible for various movements of the head, neck, and shoulders.
Anatomy of the Accessory Nerve
The accessory nerve has a complex anatomical course. It enters the skull through the jugular foramen and descends into the neck, where it travels alongside the internal jugular vein and the vagus nerve. The cranial component of the nerve joins the spinal component in the posterior triangle of the neck before branching out to innervate the trapezius and sternocleidomastoid muscles.
Within the posterior triangle of the neck, the accessory nerve is surrounded by other important structures such as the brachial plexus, which is a network of nerves that supplies the upper limb, and the external jugular vein, which drains blood from the head and neck region. The close proximity of these structures highlights the intricate nature of the accessory nerve’s path.
As the accessory nerve descends further into the neck, it passes through several layers of muscles, including the scalene muscles, which are important for neck movement and respiration. This proximity to other muscles and nerves underscores the interconnectedness of the body’s neural and musculoskeletal systems.
Role of the Accessory Nerve in Shoulder Movements
The trapezius muscle, innervated by the accessory nerve, plays a vital role in scapula movement by stabilizing and retracting the scapula. This muscle is essential for raising the arm above the head, rotating the scapula, and supporting the weight of objects held in the hand.
Additionally, the trapezius muscle contributes to maintaining proper posture by counteracting the downward pull of gravity on the shoulders. It helps to prevent slouching and promotes an upright position, which is important for overall spinal health.
On the other hand, the sternocleidomastoid muscle assists in turning the head and tilting it to the side. This muscle is responsible for various movements of the neck, such as looking over one’s shoulder or tilting the head to listen attentively.
Both the trapezius and sternocleidomastoid muscles, innervated by the accessory nerve, work in coordination to allow for a wide range of head, neck, and shoulder movements. Their proper functioning is essential for everyday activities, such as reaching for objects, driving, and participating in sports.
The Link Between Accessory Nerve and Scapula
The accessory nerve’s influence on the scapula cannot be overstated. Its innervation of the trapezius muscle enables coordinated movements of the scapula during various upper extremity activities. When the accessory nerve is injured, the functioning of the trapezius muscle can be compromised, leading to significant consequences for scapula function.
The Accessory Nerve’s Influence on Scapula
The trapezius muscle’s function in scapula movement is essential for many daily activities, including lifting, pushing, pulling, and reaching. When the accessory nerve is intact, the trapezius muscle contracts and stabilizes the scapula, enabling smooth and coordinated shoulder movements. However, when an accessory nerve injury occurs, it can result in weakened or paralyzed trapezius muscle, leading to scapular winging, limited shoulder movement, and weakness in the affected shoulder.
Scapular winging, also known as scapula alata, is a condition characterized by the protrusion of the scapula away from the ribcage. This abnormal positioning of the scapula affects the ability to raise the arm overhead and perform other movements involving the upper extremity. It can cause pain, discomfort, and functional limitations for individuals with an accessory nerve injury.
In addition to scapular winging, weakness or paralysis of the trapezius muscle can result in difficulties with maintaining shoulder stability. The trapezius muscle plays a crucial role in stabilizing the scapula against the ribcage, allowing for proper alignment and movement of the shoulder joint. When the trapezius muscle is compromised, individuals may experience instability in the shoulder, making it challenging to perform activities that require precise and controlled movements.
Furthermore, accessory nerve damage can lead to compensation patterns in other muscles surrounding the shoulder. When the trapezius muscle is weakened, other muscles, such as the deltoids and rotator cuff muscles, may try to compensate for the loss of function. This compensation can result in muscle imbalances and further increase the risk of injury in the shoulder and upper extremity.
Rehabilitation and Treatment
Rehabilitation and treatment for accessory nerve injuries focus on restoring function and minimizing the impact on scapula movement. Physical therapy plays a crucial role in the recovery process, aiming to strengthen the remaining muscles, improve range of motion, and promote proper movement patterns.
Physical therapists may use various techniques and exercises to target the affected muscles and facilitate their activation. These may include manual therapy, stretching, strengthening exercises, and neuromuscular re-education. The goal is to retrain the muscles and restore proper scapula movement, reducing pain and improving overall function.
In some cases, surgical intervention may be necessary to repair or reconstruct the damaged accessory nerve. This can help restore innervation to the trapezius muscle and improve scapula function. Surgical options may include nerve grafts, nerve transfers, or nerve decompression procedures.
It is important for individuals with accessory nerve injuries to seek early and appropriate medical intervention to optimize their chances of recovery. With proper treatment and rehabilitation, many individuals can regain function and resume their daily activities with minimal limitations.
Symptoms and Diagnosis of Accessory Nerve Injury
Recognizing the signs and symptoms of accessory nerve injury is crucial for timely diagnosis and treatment. While the specific symptoms may vary depending on the severity of the nerve damage, some common signs indicate potential injury to the accessory nerve.
Accessory nerve injury is a condition that can cause significant discomfort and functional limitations. The accessory nerve, also known as the 11th cranial nerve, plays a vital role in controlling certain muscles involved in shoulder movement. When this nerve is injured, it can lead to a range of symptoms that can greatly impact a person’s daily life.
Common Signs of Accessory Nerve Damage
Patients with accessory nerve injury may experience shoulder weakness on the affected side, making it challenging to perform simple tasks such as lifting objects or raising the arm. This weakness can be accompanied by pain or discomfort in the neck or shoulder region, further limiting the individual’s range of motion and overall quality of life.
In addition to shoulder weakness and pain, accessory nerve damage can also result in a noticeable condition called scapular winging. This occurs when the shoulder blade protrudes from the back, giving it an abnormal appearance. Scapular winging can be both physically and emotionally distressing for individuals, as it may affect their self-esteem and ability to engage in physical activities.
It is important to note that these symptoms can also be associated with other shoulder conditions, such as rotator cuff tears or nerve entrapment syndromes. Therefore, a comprehensive evaluation by a healthcare professional is necessary to determine the underlying cause and provide appropriate treatment.
Diagnostic Procedures for Nerve Injury
When an accessory nerve injury is suspected, various diagnostic procedures may be used to confirm the diagnosis and assess the extent of the damage. These procedures aim to gather detailed information about the nerve and muscle activity, aiding in the accurate diagnosis of the injury.
Imaging studies, such as X-rays, can provide valuable insights into the bony structures surrounding the affected area. They can help identify any fractures or abnormalities that may be contributing to the nerve injury. Magnetic resonance imaging (MRI) is another commonly used imaging technique that can provide detailed images of the soft tissues, including the nerves and muscles. This can help healthcare professionals visualize any potential nerve damage or compression.
In some cases, electromyography (EMG) may be performed to assess the electrical activity of the muscles. This test involves the insertion of small needles into the muscles to measure their response to nerve stimulation. By evaluating the muscle and nerve function, EMG can help determine the severity and location of the accessory nerve injury.
Consulting with a healthcare professional is crucial for appropriate diagnosis and treatment planning. They will consider the individual’s medical history, perform a thorough physical examination, and order the necessary diagnostic tests to accurately diagnose and assess the extent of the accessory nerve injury.
Consequences of Accessory Nerve Injury on the Scapula
An accessory nerve injury can have both short-term and long-term effects on scapula function, impacting the individual’s ability to perform daily activities and participate in physical endeavors.
The scapula, commonly known as the shoulder blade, is a crucial bone that plays a vital role in the movement and stability of the shoulder joint. When the accessory nerve, also known as the 11th cranial nerve, is injured, it can disrupt the normal functioning of the scapula, leading to a range of consequences.
Short-term Effects on Scapula Function
In the acute phase of an accessory nerve injury, scapula function may be severely compromised. Reduced shoulder stability, limited range of motion, and weakness in the affected shoulder and arm can significantly impair everyday activities and decrease quality of life.
Simple tasks like reaching for objects, lifting weights, or even combing one’s hair can become challenging and painful. The loss of shoulder stability can also make it difficult to perform activities that require overhead movements, such as throwing a ball or reaching for items on high shelves.
Furthermore, the weakness in the affected shoulder and arm can lead to muscle imbalances, as the surrounding muscles may compensate for the lack of strength. This compensation can potentially result in further strain and injury to other muscles and joints in the shoulder complex.
However, with appropriate treatment and rehabilitation, the short-term effects can often be minimized, leading to better outcomes in the long run. Physical therapy, exercises targeting scapular stability and strength, and other interventions can help restore normal function and alleviate the immediate impact of the injury.
Long-term Implications for the Scapula
If left untreated or inadequately rehabilitated, long-term consequences of an accessory nerve injury can manifest. Chronic scapular winging and persistent weakness in the affected shoulder may limit functional abilities, hinder participation in sports or physical activities, and negatively impact overall shoulder health.
Scapular winging refers to the abnormal protrusion or sticking out of the scapula from the back, creating an uneven appearance. This condition can occur due to the imbalance between the muscles that control scapular movement, resulting in the scapula not being properly stabilized against the ribcage.
Chronic scapular winging can lead to further complications, such as shoulder impingement syndrome, where the rotator cuff tendons become irritated and inflamed due to abnormal scapular movement. This can cause pain, limited range of motion, and difficulty in performing overhead activities.
Moreover, persistent weakness in the affected shoulder can hinder the individual’s ability to engage in physical activities and sports that require upper body strength. This can have a significant impact on their overall fitness level and participation in recreational or competitive endeavors.
Rehabilitation and ongoing management play a crucial role in mitigating the long-term implications of accessory nerve injury on scapula function. Physical therapy programs that focus on strengthening the muscles surrounding the scapula, improving scapular stability, and restoring normal movement patterns can help individuals regain functional abilities and improve their quality of life.
In conclusion, an accessory nerve injury can have both short-term and long-term consequences on scapula function. While the short-term effects can be debilitating, with appropriate treatment and rehabilitation, individuals can regain normal function and minimize the long-term implications. It is essential to seek professional medical advice and engage in a comprehensive rehabilitation program to optimize recovery and prevent further complications.
Treatment and Rehabilitation for Accessory Nerve Injury
When it comes to the treatment and rehabilitation of accessory nerve injury, early intervention is key. Consulting with a healthcare professional, such as a neurologist or an orthopedic specialist, is crucial to determine the appropriate course of action based on the specific circumstances of the injury.
Accessory nerve injury can have a significant impact on a person’s daily life, affecting their ability to perform simple tasks such as lifting objects, raising their arm, or turning their head. Therefore, it is essential to explore various treatment options to promote recovery and restore function.
Medical Interventions for Nerve Injury
In some cases, surgical intervention may be necessary to repair or reinnervate the damaged accessory nerve. Surgical options may include nerve grafting or nerve transfers, where healthy nerves from other areas of the body are used to restore function to the affected muscles. However, the suitability of surgical intervention depends on various factors, and healthcare professionals will evaluate each case individually to determine the best approach.
During nerve grafting, a section of a healthy nerve is harvested and used to bridge the gap between the damaged ends of the accessory nerve. This procedure allows for the regeneration of nerve fibers and the restoration of muscle function over time.
Nerve transfers involve taking a functional nerve from one area of the body and connecting it to the damaged accessory nerve. This technique allows for a more direct reinnervation of the affected muscles, promoting quicker recovery and improved outcomes.
While surgical interventions can be effective, they are not always the first line of treatment. Non-surgical approaches, such as physical therapy, are often recommended as initial treatment options.
Physical Therapy and Rehabilitation Techniques
Physical therapy plays a critical role in the rehabilitation of accessory nerve injuries. A skilled physical therapist will assess the individual’s specific impairments and design a comprehensive rehabilitation program tailored to their needs.
During the initial evaluation, the physical therapist will assess the individual’s range of motion, muscle strength, and functional abilities. This assessment helps identify areas of weakness or limitations that need to be addressed during the rehabilitation process.
Therapeutic exercises are a fundamental component of accessory nerve injury rehabilitation. These exercises focus on strengthening the affected muscles, improving coordination, and restoring normal movement patterns. The physical therapist will guide the individual through a series of exercises that target the specific muscles affected by the injury.
Functional training is another essential aspect of rehabilitation. This involves practicing activities that mimic real-life movements and tasks to improve the individual’s ability to perform daily activities independently. For example, if the injury affects the ability to lift objects, the physical therapist may incorporate lifting exercises into the rehabilitation program.
In addition to therapeutic exercises and functional training, manual therapy techniques may be used to address soft tissue restrictions, joint mobility issues, or muscle imbalances. These techniques, such as joint mobilizations, soft tissue mobilization, or myofascial release, can help improve overall movement and reduce pain or discomfort.
Modalities such as electrical stimulation or ultrasound may also be employed by the physical therapist to aid in the recovery process. Electrical stimulation can help stimulate muscle contractions, improve blood flow, and reduce muscle atrophy. Ultrasound, on the other hand, can promote tissue healing and reduce inflammation.
Throughout the rehabilitation process, the physical therapist will closely monitor the individual’s progress and make adjustments to the treatment plan as needed. This may involve increasing the intensity or complexity of exercises, introducing new techniques, or modifying the program based on the individual’s response to treatment.
In conclusion, the treatment and rehabilitation of accessory nerve injury require a multidisciplinary approach involving healthcare professionals, such as neurologists, orthopedic specialists, and physical therapists. Early intervention, whether through surgical or non-surgical interventions, combined with a comprehensive rehabilitation program, can significantly improve outcomes and help individuals regain function and independence.
Prevention and Management of Accessory Nerve Injury
Preventing an accessory nerve injury is not always possible, as accidents and trauma can occur unexpectedly. However, some measures can be taken to reduce the risk of injury and manage the condition effectively. It is important to note that prevention and management strategies should be discussed and implemented under the guidance of a healthcare professional.
Preventive Measures for Nerve Damage
Avoiding excessive strain on the neck and shoulders, maintaining good posture, practicing safe lifting techniques, and avoiding activities that may put excessive stress on the upper extremity can help reduce the risk of accessory nerve injury. Additionally, individuals engaged in activities that pose a higher risk of nerve injury, such as contact sports or repetitive overhead movements, should consider appropriate protective measures and professional guidance to minimize the risk.
Living with Accessory Nerve Injury: Management Strategies
Living with an accessory nerve injury requires ongoing management to optimize functioning and quality of life. Continuing with prescribed exercises and maintaining good overall physical fitness can help compensate for any residual weaknesses. Consulting with a healthcare professional is essential to develop a comprehensive management plan tailored to individual needs, as they can provide invaluable guidance on lifestyle modifications, adaptive strategies, and assistive devices that may support daily activities.
In conclusion, an accessory nerve injury can significantly impact the functioning of the scapula, affecting shoulder stability and overall upper extremity movements. Early diagnosis, appropriate treatment, and comprehensive rehabilitation are key to improving outcomes and minimizing long-term implications. If you suspect an accessory nerve injury or experience symptoms suggestive of such an injury, consult with a healthcare professional promptly for accurate diagnosis and guidance on appropriate management strategies.


