how can the spinal accessory nerve be injured in trauma
The spinal accessory nerve, also known as the cranial nerve XI, plays a crucial role in the movement and function of our neck and shoulders. Injuries to this nerve can have significant consequences, impacting a person’s ability to perform basic tasks and affecting their overall quality of life. Understanding the causes, symptoms, and treatment options for spinal accessory nerve injury is essential in providing appropriate care and support to those affected.
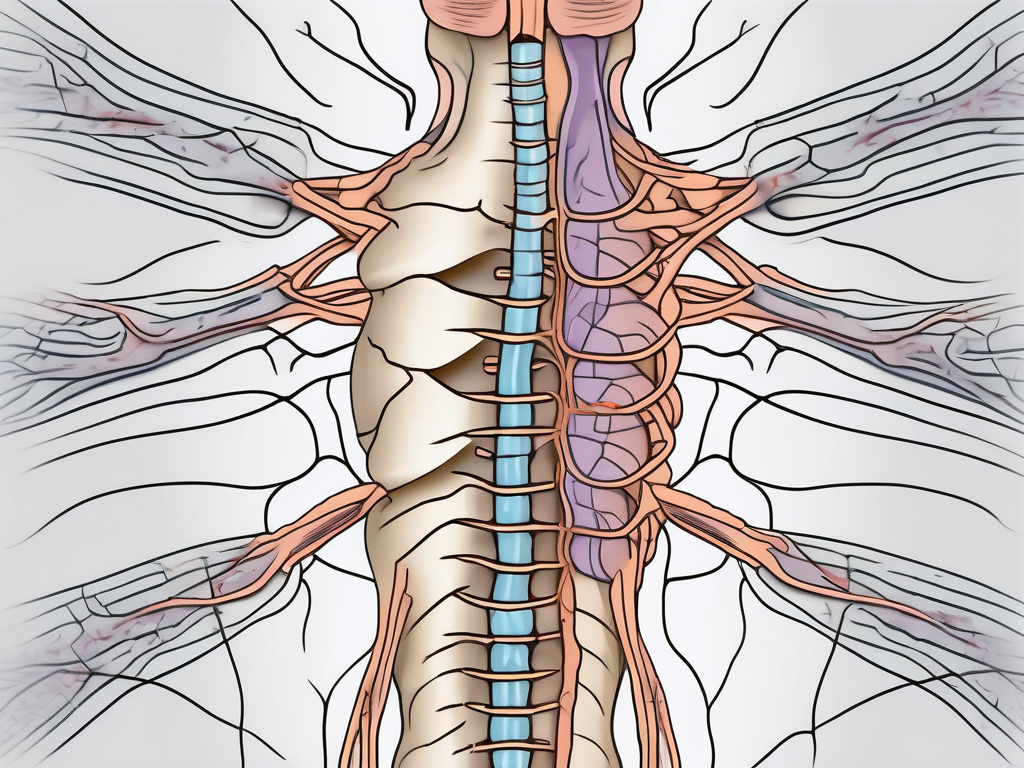
Understanding the Spinal Accessory Nerve
The spinal accessory nerve, also known as cranial nerve XI, is an important nerve that plays a crucial role in the movement and function of the neck and shoulders. It originates in the brainstem and extends down into the neck, supplying motor function to the sternocleidomastoid and trapezius muscles. These muscles facilitate a wide range of movements, including rotating the head, tilting the neck, and elevating and retracting the shoulders. Thus, any trauma or injury that affects this nerve can lead to severe limitations in movement and function.
Understanding the anatomy and function of the spinal accessory nerve is essential in diagnosing and treating conditions that may affect it. Let’s delve deeper into the intricacies of this nerve.
Anatomy of the Spinal Accessory Nerve
The spinal accessory nerve arises from the upper part of the spinal cord and travels through the skull base before branching out into the neck and shoulder regions. It is composed of both motor and sensory fibers, which allow it to transmit signals between the brain and the muscles it innervates.
As the spinal accessory nerve travels through the skull base, it passes through a small opening called the foramen magnum. This opening is located at the base of the skull and serves as a pathway for the nerve to exit the brainstem. From there, it continues its course through the neck, where it innervates the sternocleidomastoid and trapezius muscles.
The spinal accessory nerve’s intimate relationship with other vital structures, such as the jugular vein, carotid artery, and cervical lymph nodes, makes it vulnerable to both external and internal injuries. Any damage or compression to these neighboring structures can potentially affect the function of the nerve.
Function of the Spinal Accessory Nerve
The primary function of the spinal accessory nerve is to control the muscles of the neck and shoulders. It works in conjunction with other nerves, such as the facial nerve and the trigeminal nerve, to coordinate the movement of these muscles, allowing for smooth and coordinated motion.
When the spinal accessory nerve is functioning properly, it enables us to perform various activities that involve the neck and shoulders. For example, it allows us to turn our heads from side to side, tilt our necks forward and backward, and raise and lower our shoulders. These movements are essential for everyday tasks like driving, looking around, and lifting objects.
Damage to the spinal accessory nerve can disrupt the communication between the brain and the muscles it innervates, leading to various impairments. Common symptoms of spinal accessory nerve injury include weakness or paralysis of the sternocleidomastoid and trapezius muscles, resulting in difficulty in performing the aforementioned movements. Additionally, individuals with spinal accessory nerve damage may experience pain, muscle atrophy, and limited range of motion in the neck and shoulders.
Diagnosing and treating spinal accessory nerve injuries require a comprehensive evaluation by a healthcare professional, such as a neurologist or an orthopedic surgeon. Treatment options may include physical therapy, medication, and in severe cases, surgical intervention to repair or bypass the damaged nerve.
In conclusion, the spinal accessory nerve is a vital component of our nervous system, responsible for controlling the muscles of the neck and shoulders. Understanding its anatomy and function is crucial in diagnosing and managing conditions that may affect it. By gaining a deeper insight into the complexities of this nerve, we can better appreciate its role in our everyday movements and work towards preserving its health and function.
Common Causes of Spinal Accessory Nerve Injury
Spinal accessory nerve injuries can occur due to various factors. Understanding the potential causes can help individuals and healthcare professionals identify the risk factors and take appropriate precautions.
The spinal accessory nerve, also known as cranial nerve XI, is a motor nerve that controls the movement of certain muscles in the neck and shoulder. It originates from the spinal cord in the upper neck and travels through the neck and shoulder region, innervating the trapezius and sternocleidomastoid muscles. Any damage to this nerve can result in significant functional impairment.
Traumatic Injuries and Accidents
Motor vehicle accidents, falls, and sports-related injuries are common causes of traumatic spinal accessory nerve injuries. These types of accidents can involve sudden and forceful movements of the neck and shoulder, leading to direct trauma to the nerve.
For example, in a motor vehicle accident, the impact can cause the head to jerk forward or backward abruptly, straining or damaging the spinal accessory nerve. Similarly, in sports-related injuries, a fall or collision can result in a sudden twist or compression of the neck or shoulder, putting the nerve at risk.
It is important to note that the severity of the nerve injury can vary depending on the extent of the trauma. In some cases, the nerve may only be stretched or compressed, causing temporary dysfunction. However, in more severe cases, the nerve may be completely severed, requiring surgical intervention for repair.
Surgical Procedures and Risks
Surgical interventions that involve the neck or shoulder area carry the risk of inadvertent damage to the spinal accessory nerve. Procedures such as lymph node dissections or neck surgeries often require delicate maneuvering, and any unintended injury to the nerve can occur, leading to potential complications.
During these surgical procedures, the surgeon must carefully navigate around the nerve to avoid damaging it. However, due to the complex anatomy of the neck and the proximity of the nerve to other structures, such as blood vessels and lymph nodes, there is always a risk of accidental injury.
Additionally, certain patient factors, such as anatomical variations or previous surgeries in the area, can increase the likelihood of nerve injury during surgery. Surgeons must be vigilant and take necessary precautions to minimize the risk of damaging the spinal accessory nerve.
In conclusion, spinal accessory nerve injuries can occur due to traumatic accidents or surgical procedures. Understanding the potential causes and associated risks is crucial for prevention, early detection, and appropriate management of these injuries.
Symptoms and Diagnosis of Spinal Accessory Nerve Damage
Identifying the signs and symptoms of spinal accessory nerve damage is crucial for timely diagnosis and intervention. While each individual may experience different symptoms, certain common indicators may warrant further investigation.
Spinal accessory nerve damage can have a significant impact on an individual’s daily life. The symptoms can vary depending on the severity and location of the injury. In some cases, individuals may experience pain or weakness in the neck and shoulder region. This can make simple tasks such as turning the head or lifting objects extremely challenging.
One of the most noticeable physical symptoms of spinal accessory nerve damage is shoulder drooping. This occurs when the muscles responsible for lifting the shoulder become weakened or paralyzed. As a result, the affected shoulder may appear lower than the unaffected side. This can not only affect a person’s appearance but also their ability to perform certain movements.
Another common symptom is limited range of motion in the neck and shoulder. Individuals with spinal accessory nerve damage may find it difficult to rotate or tilt their head, making it challenging to perform activities that require a wide range of motion, such as driving or playing sports.
During a physical examination, healthcare professionals may also observe muscle atrophy and muscle imbalances. Muscle atrophy refers to the wasting away or loss of muscle mass due to lack of use or nerve damage. This can be seen as a noticeable decrease in the size and strength of the muscles in the affected area. Muscle imbalances, on the other hand, occur when certain muscles become weaker while others compensate and become overactive. These imbalances can further contribute to limited range of motion and difficulty in performing everyday tasks.
Diagnostic Tests and Procedures
To confirm the extent and location of spinal accessory nerve injury, healthcare professionals may employ diagnostic tests such as electromyography (EMG), nerve conduction studies, and medical imaging. These tests can provide valuable insights into the nature of the damage and help guide treatment decisions.
Electromyography (EMG) is a diagnostic procedure that involves the insertion of small needles into the muscles to measure their electrical activity. This test can help determine if the spinal accessory nerve is functioning properly and identify any abnormalities or disruptions in the nerve signals.
Nerve conduction studies are another commonly used diagnostic test for spinal accessory nerve damage. This test involves the application of small electrical shocks to the nerves and recording the speed and strength of the nerve signals. By measuring the conduction of the nerve impulses, healthcare professionals can assess the integrity of the spinal accessory nerve and identify any areas of damage or dysfunction.
In some cases, medical imaging techniques such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be used to visualize the spinal accessory nerve and surrounding structures. These imaging tests can provide detailed images of the nerves, muscles, and bones, allowing healthcare professionals to identify any structural abnormalities or lesions that may be causing the nerve damage.
Overall, a comprehensive evaluation of the symptoms and diagnostic tests is essential for an accurate diagnosis of spinal accessory nerve damage. Early detection and intervention can greatly improve the prognosis and quality of life for individuals with this condition.
Treatment Options for Spinal Accessory Nerve Injury
When it comes to treating spinal accessory nerve injuries, a multidisciplinary approach is often beneficial. Rehabilitation specialists, neurologists, and surgeons collaborate to develop a customized treatment plan tailored to the individual’s specific needs and circumstances.
Spinal accessory nerve injuries can occur due to various causes such as trauma, surgical complications, or underlying medical conditions. The severity of the injury and its impact on the patient’s daily life determine the appropriate treatment approach.
Non-Surgical Treatments
In less severe cases, non-surgical interventions may be recommended. Physical therapy plays a crucial role in the recovery process. Skilled therapists work closely with patients to develop exercise programs that focus on strengthening the affected muscles and improving range of motion.
Occupational therapy is another non-surgical treatment option that helps individuals regain their ability to perform daily activities. Therapists assist patients in developing adaptive techniques and using assistive devices to enhance their independence and quality of life.
Targeted exercises designed specifically for spinal accessory nerve injuries can help restore strength and function. These exercises may include neck and shoulder movements, stretching, and resistance training. The goal is to gradually increase the patient’s tolerance and improve their overall mobility.
In addition to physical and occupational therapy, pain management techniques may be employed to alleviate discomfort associated with the nerve injury. These techniques can range from medication management to alternative therapies such as acupuncture or transcutaneous electrical nerve stimulation (TENS).
Assistive devices, such as braces or splints, may also be recommended to support the recovery process. These devices help stabilize the affected area and provide additional support, allowing the injured nerve to heal properly.
Surgical Interventions
In cases of severe nerve damage or when conservative approaches fail to yield significant improvement, surgical interventions may be considered. The decision to undergo surgery is typically made after a thorough evaluation of the patient’s condition and a discussion of the potential risks and benefits.
Nerve repair is a surgical procedure that aims to reconnect the damaged nerve ends. This technique involves carefully suturing the nerve segments together, allowing for the regrowth of nerve fibers and restoration of function. Nerve repair is most effective when performed soon after the injury occurs.
In cases where the damaged nerve segment is too long to be repaired directly, nerve grafting may be necessary. During this procedure, a healthy nerve from another part of the body is harvested and used as a bridge to connect the damaged nerve ends. Over time, the graft integrates with the surrounding tissues, facilitating nerve regeneration and functional recovery.
Nerve transfer procedures are another surgical option for spinal accessory nerve injuries. In this technique, a healthy nerve from a nearby muscle is redirected to the paralyzed muscle. This allows for the restoration of muscle function by bypassing the injured nerve. Nerve transfers are particularly beneficial in cases where the spinal accessory nerve cannot be repaired or grafted.
Following surgical interventions, a comprehensive rehabilitation program is essential to optimize the outcomes. Physical and occupational therapy continue to play a vital role in the recovery process, helping patients regain strength, coordination, and functional abilities.
It is important to note that the success of treatment for spinal accessory nerve injuries varies from person to person. Factors such as the extent of the injury, the individual’s overall health, and their commitment to rehabilitation play significant roles in the overall outcome.
Recovery and Rehabilitation from Spinal Accessory Nerve Injury
Recovering from a spinal accessory nerve injury takes time and patience. It is a complex process that requires a comprehensive rehabilitation program to optimize outcomes and help individuals regain their independence and functionality.
When a spinal accessory nerve injury occurs, it can result in various symptoms such as weakness or paralysis of the shoulder and neck muscles. These symptoms can significantly impact an individual’s ability to perform daily activities and may cause pain and discomfort.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in the recovery and rehabilitation process for spinal accessory nerve injuries. The primary goal of physical therapy is to restore muscle function and improve range of motion.
Rehabilitation programs for spinal accessory nerve injuries often involve a combination of strengthening and stretching exercises. These exercises are designed to target the affected muscles and gradually increase their strength and flexibility. Additionally, specific techniques such as massage, manual therapy, and neuromuscular re-education may be incorporated to promote optimal recovery.
During physical therapy sessions, individuals may work with a variety of equipment and tools to aid in their rehabilitation. This can include resistance bands, weights, and therapeutic devices that help stimulate muscle activity and improve coordination.
Physical therapists closely monitor the progress of individuals undergoing rehabilitation for spinal accessory nerve injuries. They adjust the treatment plan as needed to ensure that the exercises and techniques are appropriate and effective for each individual’s specific needs.
Long-Term Prognosis and Quality of Life
The long-term prognosis for individuals with spinal accessory nerve injuries can vary depending on the severity and location of the damage. With appropriate treatment and diligent rehabilitation, many individuals can achieve significant functional improvement and return to their activities of daily living.
However, it is important to note that each case is unique, and long-term outcomes may differ. Factors such as the extent of the nerve damage, the individual’s overall health, and their commitment to rehabilitation can all influence the final outcome.
In some cases, individuals may experience residual weakness or limitations even after completing a comprehensive rehabilitation program. However, this does not mean that they cannot lead fulfilling lives. Adaptive strategies and assistive devices can be used to compensate for any remaining deficits and help individuals maintain their independence and quality of life.
It is essential for individuals with spinal accessory nerve injuries to work closely with their healthcare team and follow a long-term management plan. This may include regular follow-up appointments, ongoing physical therapy, and lifestyle modifications to prevent further injury and promote overall well-being.
Overall, while recovering from a spinal accessory nerve injury can be challenging, with the right support and rehabilitation, individuals can make significant progress and regain a sense of normalcy in their lives.
Prevention of Spinal Accessory Nerve Injury
While not all instances of spinal accessory nerve injury can be prevented, certain measures can help reduce the risk of such injuries.
Safety Measures and Precautions
Adhering to safety guidelines and using protective equipment during sports or physical activities can minimize the risk of trauma to the neck and shoulders. Additionally, maintaining good posture, avoiding heavy backpacks or shoulder bags, and practicing safe driving habits can also contribute to injury prevention.
Importance of Early Diagnosis and Treatment
Early diagnosis and prompt treatment are crucial in optimizing outcomes for spinal accessory nerve injuries. Seeking medical attention at the first sign of symptoms or after significant trauma is crucial. A healthcare professional experienced in nerve injuries can conduct the necessary evaluations and recommend appropriate interventions.
In conclusion, understanding how the spinal accessory nerve can be injured in trauma is vital in recognizing and addressing potential complications. From anatomy and function to treatment options and prevention strategies, staying informed empowers individuals to take appropriate action and seek professional guidance when needed. If you suspect any spinal accessory nerve injury or experience concerning symptoms, consult a healthcare professional with expertise in this field for a comprehensive evaluation and appropriate care.


